More than 150 veteran healthcare facilities architects assembled in Chicago recently for the joint Summer Leadership Summit of the American College of Healthcare Architects and the AIA Academy of Architecture for Health. The topic on everyone’s mind, of course, was how the Affordable Care Act would impact healthcare design and construction––and whether the law would even make it past the coming election cycle.
Lessons in cost savings from the Geisinger Clinic
Robert W. Davies, Chief Support Services Officer at Geisinger Health System, kicked off the program with a report on the impact of healthcare reform on facilities planning.
Geisinger Health System, founded in rural Danville, Pa., in 1915, has more than 18,000 employees, of whom about a thousand are salaried physicians who provide medical care at 65 clinic sites.
Along with the Mayo and Cleveland Clinics, Geisinger was held up by the Obama Administration as a poster child for “accountable care organizations” in the run-up to the passage of the Affordable Care Act.
Among Geisinger’s recent healthcare delivery innovations, Davies cited its branded provencare program, which offers a warranty to cardiac surgery patients. A related program provides extensive follow-up care for chronic disease patients, such as those with diabetes.
As for its capital construction program, Geisinger Health has 1,600 beds in 288 buildings, totaling six million square feet. In anticipation of healthcare reform, the clinic has developed a strategic facilities plan to keep costs in line, Davies said. Among its components:
- All properties will be owned; leases will be a thing of the past.
- Standardization––of office equipment, exam rooms, signage, space standards, and clinic design––is being fiercely implemented.
- Operating expenses are being trimmed through the use of co-generation systems, chilled water storage, and isolation cleaning systems. The latter use vaporized hydrogen peroxide or UV systems to clean patient rooms and thereby help control hospital-caused infections.
- Nonclinical functions and staff are being moved off the main campus. “The IT people insisted that they had to be on campus, but we convinced them that they could do fine two or three miles away,” said Davies.
Geisinger expects to make substantial routine infrastructure improvements, investing $8.1 million in “risk operations” improvements, Davies said. The health provider currently allocates $1.35/sf a year for routine infrastructure improvements; Davies said he hopes to reach the goal of $2.00/sf per year.
Davies said he and his staff of 40 FTE facility specialists (including three architects) have been concentrating on increasing the reliability of facilities and equipment. For example, the clinic stocks spare transformers and engines, just in case they’re needed. And many of Geisinger’s old masonry buildings have been treated to façade restorations to keep them functioning properly.
Davies said his team has used Procore project management software (www.procore.com) to great effect. “It’s one of the best buys we ever made,” he told the Summit audience.
As for sustainability, Davies said, “We don’t make a big deal about it. We insist on quality materials, but nothing over the top.”
Yet not even Geisinger is perfect. A review of its facilities practices by construction manager Gilbane led to 84 positive recommendations for improvement, which Davies said he and his staff are acting on.
Futurecare: It's all about consolidation, profitability
The healthcare landscape will become more tightly controlled by large organizations, according to Fred Hessler, Director, Citigroup Health Care Group. More nonprofit systems will convert parts or all of their operations to for-profit entities, and many smaller hospitals and systems will be swallowed up by megasystems––and private investors––with greater access to capital, which they are getting at “extremely low rates,” said Hessler.
He cited several examples of this trend:
- Two years ago, Cerberus Capital Management, a private equity firm in New York, acquired Caritas Christi, a six-hospital Roman Catholic system in Boston, for $830 million, and converted it to for-profit.
- Last year, private equity firm Oak Hill Capital Partners formed a partnership with Ascension Health Care Network, the largest Catholic healthcare system in the U.S. They are currently on the hunt to gobble up several Catholic systems in New Jersey.
- Last April, Health Management Associates, an operator of acute-care hospitals, established a joint venture with Integris Health to operate five rural hospitals in Oklahoma. HMA will own an 80% controlling stake in each hospital.
- Duke Health, based in Durham, N.C., formed a joint venture with lifepoint, an administrator of rural hospitals, and is now trying to plant the Duke lifepoint flag as far afield as Marquette, Mich.
Hessler said the reason for this trend is simple: Large healthcare organizations have proven to be more profitable than small ones, primarily because they can control costs more effectively.
He said megasystems of $5 billion or more in revenue produced operating margins of 4.7%, compared to 2.0% for hospital systems with less than $1 billion in revenue. In fact, the top seven for-profit systems had an average operating margin of 9.4%.
“Investors are going into partnerships with not-for-profits because nonprofits are 80% of the market,” he said. “That’s $2.6 trillion, and they smell the money.”
Digesting the data load
Lawrence Hanrahan, MD, a partner in the health industry practice of pwc, described the huge demand for data collection and storage that awaits healthcare providers.
The cost of electronic medical records could run $100 million per hospital, yet barely half of pwc’s clients have reached Stage 3 of their PACS (picture archiving and communications systems) requirements. That’s on top of another $63 million per hospital for other data-related systems, including health information exchange and ICD-10 compliance.
Data security and disaster recovery are additional frightening concerns. “Hospitals need to have their data centers a hundred miles away, in case of disaster,” he said.
Looking at hospitals from a systems perspective, Hanrahan said Building Teams need to work with healthcare clients to:
- Lead risk management and security audits of medical equipment and building systems
- Integrate medical equipment and building systems with hospitals’ clinical, financial, and research platforms
- Identify revenue-generating reuse of vacated facilities and spaces
Data analysis capabilities (along with alignment of physician staffs) will be critical to success in a future healthcare environment that will pay for value, not volume.
Hanrahan said there’s gold in all the data healthcare systems are collecting, but they’re just not mining it. “Our clients have not caught up with the fact that information technology is an enabler, just like facilities,” he said.
How best to serve veterans
How the Veterans Administration can most effectively meet the needs of its clients was the subject of a talk by Thom Kurmel, DDES, AIA, President, TDK Consulting LLC. According to Kurmel, the VA faces a gap of $3.6 billion to “correct” conditions in its facilities. The agency’s annual construction budget is about $1.2 billion; it is estimated to have a shortfall of 42 million sf of healthcare-related space.
One of the VA’s biggest problems is how to provide care, especially long-term care, for the 40% of veterans who live at great distance from VA care facilities.
Regional cost variation is another problem. For example, New England, which will lose 40,000 veterans over the next 10 years, has a cost per patient of $8,900 a year, compared to $5,600 per patient per year in Texas.
To tackle these problems, the VA is adopting several cost-saving tactics: telemedicine (for imaging, home health, and rehabilitation), extended hours at existing care sites, and contract care in rural areas through community-based outpatient clinics. Kurmel, a retired Army colonel, reminded his audience that none of these involved the construction of new facilities.
With regard to its construction projects, Kurmel noted that the Department of Veterans Affairs is extending the use of BIM, lean construction, and integrated project delivery. The VA is also coupling its master planning process to post-occupancy evaluations in order to measure outcomes and performance more accurately, he said.
Kurmel praised the VA’s Strategic Capital Investment Planning system as a “milestone” in federal planning efforts. SCIP uses pair-wise comparison software (from Decision Lens; www.decisionlens.com) to make what Kurmel described as a “very scientific” analysis of budget needs. “SCIP has set the bar for the VA as to what they will ask [in funding] from Congress,” he said.
So, will ‘Obamacare’ still be around after November 6?
Lawyers from Drinker Biddle & Reath––Julie Scott Allen, Government Relations Director, and Anna Howard, Medicare & Health Policy Director––projected various scenarios for what might happen to the Affordable Care Act after the upcoming election.
Could a President Romney actually kill the Affordable Care Act? What if President Obama is reelected but loses control of one or both Houses of Congress? Will the 33 million uninsured Americans get coverage in 2014? What if most of the states opt out of the Medicaid exchanges?
The consensus among presenters and attendees at the ACHA/AAH Summer Leadership Summit was that, no matter the outcome of the Presidential and Congressional races, healthcare reform is not going away. Traditional “fee-for-service” medicine will have to give way to a performance-based model. According to pwc’s Hanrahan, the majority of physicians in the U.S.––58%––say they are interested in being more closely integrated with their hospitals in such an effort.
But with one of every five dollars of the country’s GDP going to the medical sector, costs have to be brought down––and the healthcare design and construction industry is going to have to play its part in that effort. +
Related Stories
Architects | Apr 24, 2024
Shepley Bulfinch appoints new Board of Director: Evelyn Lee, FAIA
Shepley Bulfinch, a national architecture firm announced the appointment of new Board of Director member Evelyn Lee, FAIA as an outside director. With this new appointment, Lucia Quinn has stepped down from the firm’s Board, after serving many years as an outside board advisor and then as an outside director.
ProConnect Events | Apr 23, 2024
5 more ProConnect events scheduled for 2024, including all-new 'AEC Giants'
SGC Horizon present 7 ProConnect events in 2024.
75 Top Building Products | Apr 22, 2024
Enter today! BD+C's 75 Top Building Products for 2024
BD+C editors are now accepting submissions for the annual 75 Top Building Products awards. The winners will be featured in the November/December 2024 issue of Building Design+Construction.
Laboratories | Apr 22, 2024
Why lab designers should aim to ‘speak the language’ of scientists
Learning more about the scientific work being done in the lab gives designers of those spaces an edge, according to Adrian Walters, AIA, LEED AP BD+C, Principal and Director of SMMA's Science & Technology team.
Resiliency | Apr 22, 2024
Controversy erupts in Florida over how homes are being rebuilt after Hurricane Ian
The Federal Emergency Management Agency recently sent a letter to officials in Lee County, Florida alleging that hundreds of homes were rebuilt in violation of the agency’s rules following Hurricane Ian. The letter provoked a sharp backlash as homeowners struggle to rebuild following the devastating 2022 storm that destroyed a large swath of the county.
Mass Timber | Apr 22, 2024
British Columbia changing building code to allow mass timber structures of up to 18 stories
The Canadian Province of British Columbia is updating its building code to expand the use of mass timber in building construction. The code will allow for encapsulated mass-timber construction (EMTC) buildings as tall as 18 stories for residential and office buildings, an increase from the previous 12-story limit.
Standards | Apr 22, 2024
Design guide offers details on rain loads and ponding on roofs
The American Institute of Steel Construction and the Steel Joist Institute recently released a comprehensive roof design guide addressing rain loads and ponding. Design Guide 40, Rain Loads and Ponding provides guidance for designing roof systems to avoid or resist water accumulation and any resulting instability.
Building Materials | Apr 22, 2024
Tacoma, Wash., investigating policy to reuse and recycle building materials
Tacoma, Wash., recently initiated a study to find ways to increase building material reuse through deconstruction and salvage. The city council unanimously voted to direct the city manager to investigate deconstruction options and estimate costs.
Student Housing | Apr 19, 2024
$115 million Cal State Long Beach student housing project will add 424 beds
A new $115 million project recently broke ground at California State University, Long Beach (CSULB) that will add housing for 424 students at below-market rates. The 108,000 sf La Playa Residence Hall, funded by the State of California’s Higher Education Student Housing Grant Program, will consist of three five-story structures connected by bridges.
Construction Costs | Apr 18, 2024
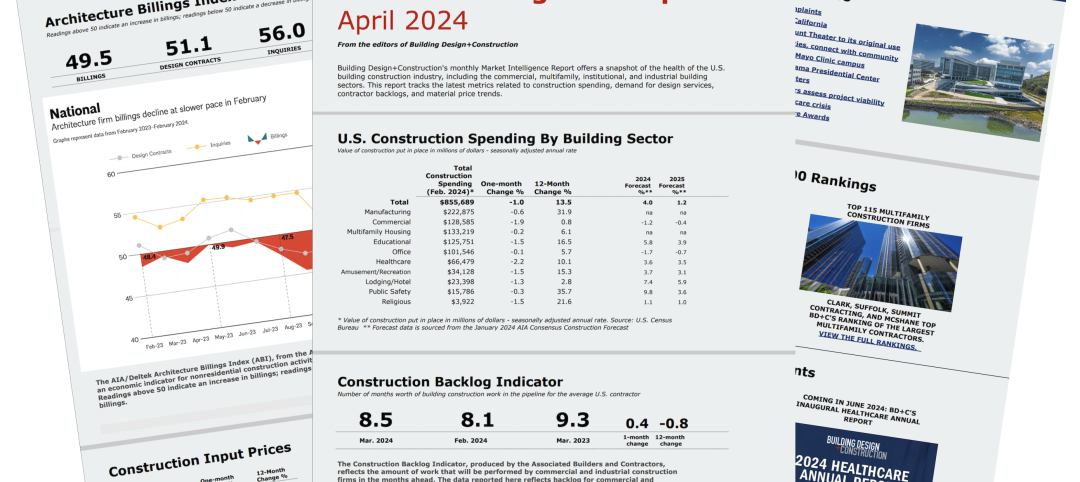
New download: BD+C's April 2024 Market Intelligence Report
Building Design+Construction's monthly Market Intelligence Report offers a snapshot of the health of the U.S. building construction industry, including the commercial, multifamily, institutional, and industrial building sectors. This report tracks the latest metrics related to construction spending, demand for design services, contractor backlogs, and material price trends.