“Innovation” was the byword as 175 healthcare designers gathered in Chicago for the American College of Healthcare Architects/AIA Academy of Architecture for Health Summer Leadership Summit.
Experts from Kaiser Permanente, Cleveland Clinic, Mayo Clinic, Massachusetts General Hospital, and other healthcare institutions and think tanks described various models they’re using to spur innovation and improve the quality of care for their patients.
That’s a topic of mounting importance under the Affordable Care Act, which can penalize a hospital with a poor record of patient satisfaction and outcomes.
KAISER PERMANENTE. Jennifer Liebermann, Co-founder of Kaiser Permanente’s 37,000-sf Garfield Innovation Center, described a typical problem such in-house innovation facilities tackle: how to reduce medication errors. “Nurses get interrupted all the time when they’re trying to give patients their meds,” she said. That leads to medication errors and injury to patients.
HOW TO DESIGN A HEALTHCARE INNOVATION CENTER
Larry Stofko, EVP of the Innovation Institute, provided ACHA/AAH summiteers with advice on designing physical spaces to enable innovation:
1. Make the space flexible, with movable walls and furnishings.
2. Make it inspiring, with whimsical artwork and “creative” colors (orange and blue seem to work best).
3. Make it collaborative, with lots of whiteboards, wall space, and glass to write on.
4. Make it social, with a working kitchen, comfy couches, springboard chairs.
5. Make it hard-working, by providing the right tools and hardware (e.g., 3D printers).
6. Make sure it reflects the institution’s culture and brand.
7. Provide a dedicated showcase to display your innovation successes.
The Garfield Center team tried several ideas, even something that looked like a hazmat suit (“We tested it on nurses, and they said they’d never wear that thing,” said Liebermann). The solution: a bright yellow sash that the nurse wears over her shoulder when dispensing prescriptions.
“That sash lets everyone know, ‘Don’t interrupt me, I’m dispensing meds,’” said Liebermann. A simple and inexpensive solution, but so effective that it’s being rolled out through the entire 32-hospital Kaiser Permanente system.
“We borrow ideas from other healthcare organizations, but some of our most powerful inspiration comes from outside healthcare,” said Liebermann. KP is working with Walmart on telemedicine and with NASA on improving safety in operating rooms. “NASA has a lot of experience with its people working in tight spaces,” she said.
CLEVELAND CLINIC is an institution with a long history of innovation in healthcare—2,600 patent applications, 450 royalty licenses, 71 spinoffs, $799 million in equity investments, according to Brian Kolonick, General Manager of Cleveland Clinic Innovations’ Global Healthcare Innovations Alliance. The alliance includes MedStar Health, North Shore–LIJ, Promedica, the University of Notre Dame, and Marshfield Clinic.
Half (50%) of the clinic’s inventions have been medical devices, along with IT solutions (23%) and therapeutic/diagnostic systems (22%). The remaining 5% were healthcare delivery solutions. “Delivery solutions are our secret sauce,” said Kolonick. Cleveland Clinic excels at coming up with new ways to improve patient outcomes and then outsourcing those capabilities to other institutions.
Cleveland Clinic is not modest about collaborating with the private sector and government agencies. It’s working with NASA Glenn Research Center to see how lessons from space medicine can be applied to terrestrial healthcare. They’re consulting with Parker Hannifan (“They know a lot about tubes, and we use a lot of tubes in healthcare,” said Kolonick) and Lubrizol, for its expertise in polymers.
“We’re also involved with Cox Communications, to see how they can help us work with patients from inside the home, or via healthcare pods at the grocery store,” he said.
MAYO CLINIC’s Center for Innovation was founded in 2008. “We’re a shared service for innovation across Mayo,” said Barbara Spurrier, MHA, CMPE, the CFI’s Administrative Director. Its staff of 60 includes scientists, designers, programmers, analysts, bioethicists, nurses, and lawyers.
The CFI has 47 projects in the works, most of which have to be completed in 12 months. “There are a lot of things that don’t work out,” Spurrier said. “Sometimes we get all the way to a prototype and it doesn’t work, and we have to put it on the shelf.”
Mayo is looking at developing smartphone apps, such as one that teenage asthma patients could use to monitor their condition without having to go to the clinic.
Video medical visits, perhaps via Skype, are of keen interest to Mayo, especially for use with older patients. “How can we help seniors thrive in place?” asked Spurrier. “We know that 85% of them can get their care at home. What conditions need to be in place so that we can serve them right in their homes?”
“The Garage” is another Mayo innovation initiative—an incubator for products and services with commercialization potential. There’s also CoDE, which provides as much as $50,000 each to up to 10 teams a year for what Spurrier called “open innovation.” Mayo’s “Transform” international symposium recently attracted 850 innovators from 16 countries.
Mayo’s newest project: the 7,000-sf Well Living Lab, in collaboration with its home city of Rochester, Minn. “We’ll be looking at the intersection of medical and scientific research as related to the built environment,” said Spurrier.
MASS GENERAL. James A. Gordon, MD, MPA, Director of the Learning Laboratory at Massachusetts General Hospital and the Gilbert Program in Medical Simulation at Harvard Medical School, emphasized the need for simulation tools and labs at teaching hospitals. He said simulation training was crucial to improving patient safety and accelerating and assuring physician expertise.
“In medicine, every day is game day,” said Gordon, an emergency medicine specialist. To his fellow physicians, he posed this rhetorical question: “Can you continue to maintain your standards without allocating time for being offline to train?” Gordon didn’t say so outright, but it was clear he didn’t think so.
Related Stories
Healthcare Facilities | Dec 7, 2023
New $650 million Baptist Health Care complex opens in Pensacola
Baptist Health Care’s new $650 million healthcare complex opened recently in Pensacola, Fla. Featuring a 10-story, 268-bed hospital, the project “represents the single-largest investment in the healthcare history of northwest Florida,” said Gresham Smith project executive Robert “Skip” Yauger, AIA, LEED AP. The 602,000 sf Baptist Hospital is equipped with a Level II trauma center that provides 61 exam rooms and three triage areas.
Engineers | Nov 27, 2023
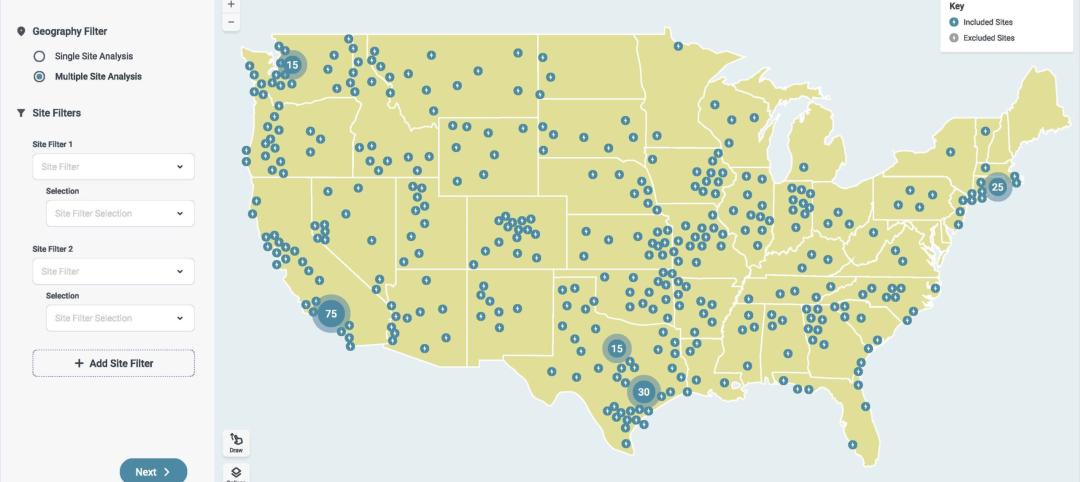
Kimley-Horn eliminates the guesswork of electric vehicle charger site selection
Private businesses and governments can now choose their new electric vehicle (EV) charger locations with data-driven precision. Kimley-Horn, the national engineering, planning, and design consulting firm, today launched TREDLite EV, a cloud-based tool that helps organizations develop and optimize their EV charger deployment strategies based on the organization’s unique priorities.
Healthcare Facilities | Nov 3, 2023
The University of Chicago Medicine is building its city’s first freestanding cancer center with inpatient and outpatient services
The University of Chicago Medicine (UChicago Medicine) is building Chicago’s first freestanding cancer center with inpatient and outpatient services. Aiming to bridge longstanding health disparities on Chicago’s South Side, the $815 million project will consolidate care and about 200 team members currently spread across at least five buildings. The new facility, which broke ground in September, is expected to open to patients in spring 2027.
Sponsored | | Oct 17, 2023
The Evolution of Medical Facility Security
As the healthcare system grows, securing these facilities becomes ever more challenging. Increasingly, medical providers have multiple facilities within their networks, making traditional keying systems and credentialing impractical.
Healthcare Facilities | Oct 11, 2023
Leveraging land and light to enhance patient care
GBBN interior designer Kristin Greeley shares insights from the firm's latest project: a cancer center in Santa Fe, N.M.
Healthcare Facilities | Oct 9, 2023
Design solutions for mental health as a secondary diagnosis
Rachel Vedder, RA, LEED AP, Senior Architect, Design Collaborative, shares two design solutions for hospitals treating behavioral health patients.
Giants 400 | Oct 5, 2023
Top 115 Healthcare Construction Firms for 2023
Turner Construction, Brasfield & Gorrie, JE Dunn Construction, DPR Construction, and McCarthy Holdings top BD+C's ranking of the nation's largest healthcare sector contractors and construction management (CM) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report. Note: This ranking includes revenue related to all healthcare buildings work, including hospitals, medical office buildings, and outpatient facilities.
Giants 400 | Oct 5, 2023
Top 90 Healthcare Engineering Firms for 2023
Jacobs, WSP, IMEG, BR+A, and Affiliated Engineers head BD+C's ranking of the nation's largest healthcare sector engineering and engineering/architecture (EA) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report. Note: This ranking includes revenue related to all healthcare buildings work, including hospitals, medical office buildings, and outpatient facilities.
Giants 400 | Oct 5, 2023
Top 175 Healthcare Architecture Firms for 2023
HDR, HKS, CannonDesign, Stantec, and SmithGroup top BD+C's ranking of the nation's largest healthcare sector architecture and architecture/engineering (AE) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report. Note: This ranking includes revenue related to all healthcare buildings work, including hospitals, medical office buildings, and outpatient facilities.
Adaptive Reuse | Sep 19, 2023
Transforming shopping malls into 21st century neighborhoods
As we reimagine the antiquated shopping mall, Marc Asnis, AICP, Associate, Perkins&Will, details four first steps to consider.