The use of third parties to develop and own new medical real estate projects is increasingly viewed as an attractive option for health systems seeking ways to preserve and generate precious capital resources to fund acute care programs and market share growth. The right third-party developer can help health systems create medical facilities with market-competitive rental rates as well as provide several benefits, such as future flexibility for the hospital, avoidance of the legal exposure that may come with serving as a landlord to referring physicians, and a potential investment vehicle for physician-tenants.
However, the selection of a developer for a new project can create challenges for health system executives. To obtain the most competitive terms, hospitals usually issue a request for proposal (RFP) as part of the selection process. In addition to the time and effort dedicated to developing and managing the RFP, hospitals also may face challenges in keeping pace with the changing economics of the real estate development industry.
One of the biggest challenges health systems face when issuing a RFP is in maintaining maximum negotiating leverage for as long as possible when selecting a developer for a new project. Three critical steps can enhance the negotiating leverage of health systems when managing the developer selection process: understanding the risk-return profile of the equity backing the developer, establishing confidence in the developer's ability to achieve target value design, and diligently vetting all legal documentation associated with the project.
UNDERSTANDING THE EQUITY
A health system increases its likelihood of negotiating the best terms for a new project by understanding the dynamic of the equity source behind a developer. Although the demand for healthcare development projects among equity sources has significantly increased in recent years, the number of opportunities to place the equity remains below prerecession levels. The healthcare development market peaked in 2008 with $40.4 billion in private U.S. healthcare construction spending, and it remains 23 percent below that, at $31 billion, as of November 2015.
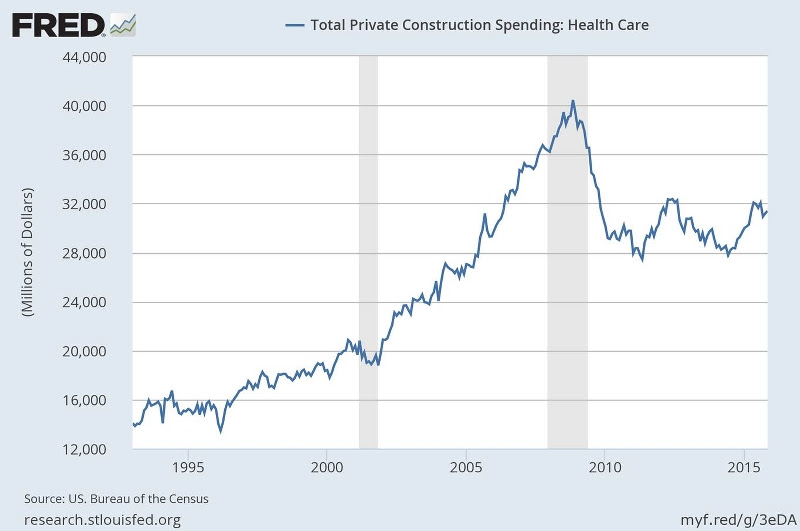 Total Private Construction Spending: Health Care
Total Private Construction Spending: Health Care
In a market with limited opportunities to place capital, low interest rates, and an abundance of debt and equity that is pursuing healthcare real estate, developer yields continue to compress for the most competitive projects, to the point that healthcare developers are much less likely to fund new projects through investment from "friends and family." Instead, developers looking to compete are seeking the most aggressive sources of capital, which typically take the form of equity from pension funds and publicly traded real estate investment trusts (REITs).
Although pension funds have the lowest cost of capital in today's market, their commitments to new projects are closely tied to the geographic location of the project and the credit of the health system. The most active state pension funds with allocations to healthcare real estate, usually advised through investment managers, include those in Alaska, Arizona, Kentucky, Massachusetts, Michigan, New Jersey, Wisconsin and
Texas. As public pensions shift their asset allocation toward the "endowment model," which historically has had higher allocations in alternative assets, we expect this capital source to correspondingly increase allocations to commercial real estate. Pension funds are primarily seeking real estate development opportunities, including through health systems that are in primary and secondary markets with backing by investment-grade credit. Although pension funds may have very specific criteria, they typically are able to offer greater flexibility regarding forward equity commitments, ground lease structuring, and purchase options by the hospital sponsor, and ownership models for physician tenants.
Although public REITs have less flexibility than pension fund equity, they typically offer longer term stability. REITs, as an asset class, generally do not sell their owned facilities because each asset in their portfolio provides rental income that supports the payout of dividends to their shareholders. As a potentially infinite holder of real estate, REITs historically have served as a preferred equity source for health systems. However, REITs are more interest-rate sensitive than any other equity source for developers, and generally are unable to offer a fixed forward equity commitment more than 12 months in advance for any project. REIT stock prices tend to move counter to fixed-income interest rates, such as the 10-year Treasury note. As interest rates decrease, stock prices for REITs tend to increase because they pay investor dividends, which typically float between 4 and 5 percent. Investors faced with rising interest rates tend to move away from dividend-generating stocks and toward options with higher yields.
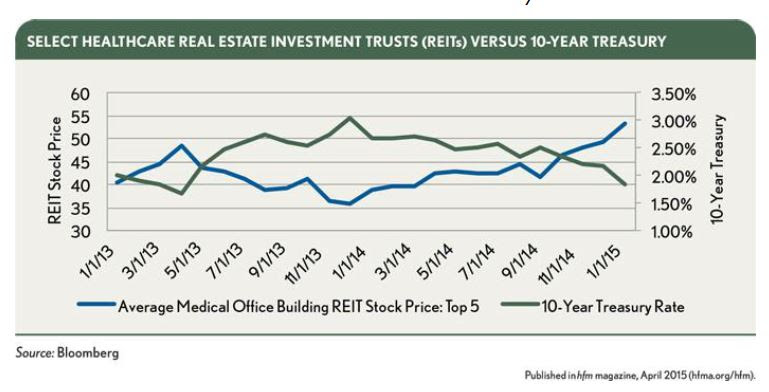 Select Healthcare REITs Versus 10-Year Treasury
Select Healthcare REITs Versus 10-Year Treasury
BALANCING COSTS WITH DESIGN
During the developer proposal selection process, health systems should beware that the lowest yield does not always produce the lowest lease rate. Health systems typically emphasize the lease constant or developer yield, but pay less attention to the other variables in the equation, such as the cost of construction or miscellaneous fees.
A key question health systems should ask is whether the developer is experienced in achieving target value design (TVD) while delivering a state-of-the art facility. TVD delivers value to the health system through the design process while recognizing the importance of constraints such as construction costs. TVD was a target-costing practice popularized in Japan during the economically turbulent 1990s to create high-quality, cost-efficient facilities. The process aims to push the developer, architect, and general contractor to excel and innovate through the exclusion of standard approaches to design and construction. The use of financial targets and consideration of the expected value to the health system can drive creativity and problem solving. Developers often do not select their architect or general contractor before submitting their proposal to ensure that the hospital helps in the selection process for those positions and supports them. Hospitals can enhance their standard role in the selection process by reviewing a short list of the developer's proposed architects and general contractors to help gauge their historical success in achieving TVD.
As part of the selection process, health systems can go beyond simply analyzing the developer's fee by comparing miscellaneous fees, such as those for feasibility studies, project management, leasing, and financing. When miscellaneous fees surface after the developer is selected, the overall budget is increased, leaving the health system to ultimately grapple with a higher rental rate.
INVOLVING LEGAL EXPERTISE EARLY
Before beginning the developer selection process, health systems should determine their priorities. A memorandum of understanding should clearly state preferences regarding issues such as future options to purchase the facility, rights of first refusal to lease the space, specific ground-lease control provisions, and physician ownership models. The health system should share this document with the short list of developers in the final round of the selection process, and should request redline comments from the developer's legal counsel. At this point in the selection process, the involved parties generally are provided with key legal documents, such as the developer agreement, ground lease (if applicable), and space lease, to make a final selection. Although the developer may formally present the proposal, the legal documents often are provided for comment to the equity source backing the developer. A critical step is for the health system to review redline comments while it still has leverage, to bolster its negotiating position if the equity source responds with any comments that conflict with the health system's goals.
CONCLUSION
By running a detailed and competitive process from the beginning while in a position of leverage, a health system can benefit from a more streamlined process and from minimized risk after selecting a developer for a new project.
Footnote
a. Lease Constant: The developer and tenant agree on a factor (called a lease constant or developer yield) to be multiplied by the total development cost of the project to determine the initial annual rent. For example, if the lease constant/developer yield is 9 percent and the project cost for a 75,000-square-foot medical office building is $20 million, then the initial rent would be $1.8 million, or $24 per square foot.
About the Author: Chris Bodnar joined CBRE in 2003 and is an Executive Vice President of the Investment Properties division and co-leads the CBRE Healthcare Capital Markets Group with his business partner Lee Asher. Disciplined in the specialty of Investment Sales, Mr. Bodnar has been involved in the disposition of over 10 million square feet of commercial assets, exceeding a total value of $3 billion dollars on behalf of his clients since 2010.
Related Stories
Healthcare Facilities | Dec 7, 2023
New $650 million Baptist Health Care complex opens in Pensacola
Baptist Health Care’s new $650 million healthcare complex opened recently in Pensacola, Fla. Featuring a 10-story, 268-bed hospital, the project “represents the single-largest investment in the healthcare history of northwest Florida,” said Gresham Smith project executive Robert “Skip” Yauger, AIA, LEED AP. The 602,000 sf Baptist Hospital is equipped with a Level II trauma center that provides 61 exam rooms and three triage areas.
Engineers | Nov 27, 2023
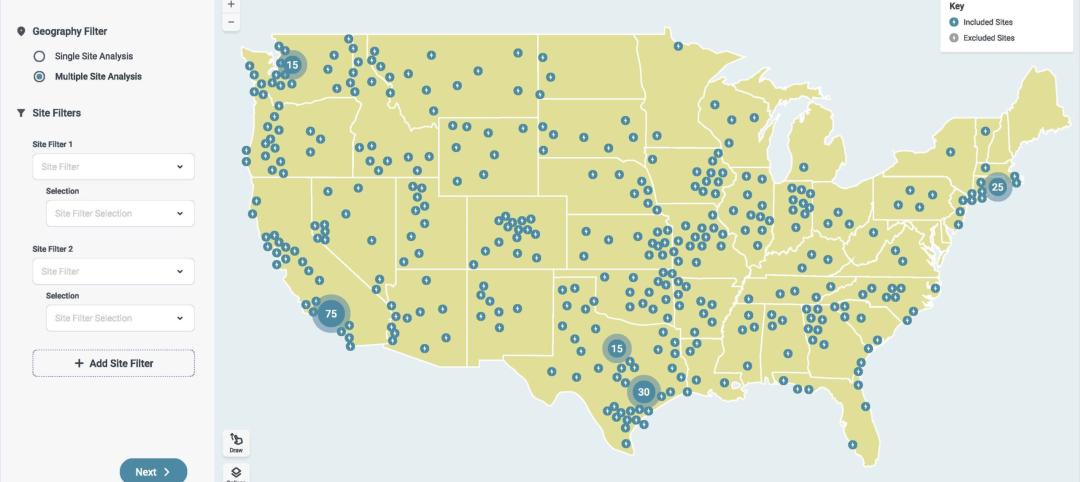
Kimley-Horn eliminates the guesswork of electric vehicle charger site selection
Private businesses and governments can now choose their new electric vehicle (EV) charger locations with data-driven precision. Kimley-Horn, the national engineering, planning, and design consulting firm, today launched TREDLite EV, a cloud-based tool that helps organizations develop and optimize their EV charger deployment strategies based on the organization’s unique priorities.
Healthcare Facilities | Nov 3, 2023
The University of Chicago Medicine is building its city’s first freestanding cancer center with inpatient and outpatient services
The University of Chicago Medicine (UChicago Medicine) is building Chicago’s first freestanding cancer center with inpatient and outpatient services. Aiming to bridge longstanding health disparities on Chicago’s South Side, the $815 million project will consolidate care and about 200 team members currently spread across at least five buildings. The new facility, which broke ground in September, is expected to open to patients in spring 2027.
Sponsored | | Oct 17, 2023
The Evolution of Medical Facility Security
As the healthcare system grows, securing these facilities becomes ever more challenging. Increasingly, medical providers have multiple facilities within their networks, making traditional keying systems and credentialing impractical.
Healthcare Facilities | Oct 11, 2023
Leveraging land and light to enhance patient care
GBBN interior designer Kristin Greeley shares insights from the firm's latest project: a cancer center in Santa Fe, N.M.
Healthcare Facilities | Oct 9, 2023
Design solutions for mental health as a secondary diagnosis
Rachel Vedder, RA, LEED AP, Senior Architect, Design Collaborative, shares two design solutions for hospitals treating behavioral health patients.
Giants 400 | Oct 5, 2023
Top 115 Healthcare Construction Firms for 2023
Turner Construction, Brasfield & Gorrie, JE Dunn Construction, DPR Construction, and McCarthy Holdings top BD+C's ranking of the nation's largest healthcare sector contractors and construction management (CM) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report. Note: This ranking includes revenue related to all healthcare buildings work, including hospitals, medical office buildings, and outpatient facilities.
Giants 400 | Oct 5, 2023
Top 90 Healthcare Engineering Firms for 2023
Jacobs, WSP, IMEG, BR+A, and Affiliated Engineers head BD+C's ranking of the nation's largest healthcare sector engineering and engineering/architecture (EA) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report. Note: This ranking includes revenue related to all healthcare buildings work, including hospitals, medical office buildings, and outpatient facilities.
Giants 400 | Oct 5, 2023
Top 175 Healthcare Architecture Firms for 2023
HDR, HKS, CannonDesign, Stantec, and SmithGroup top BD+C's ranking of the nation's largest healthcare sector architecture and architecture/engineering (AE) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report. Note: This ranking includes revenue related to all healthcare buildings work, including hospitals, medical office buildings, and outpatient facilities.
Adaptive Reuse | Sep 19, 2023
Transforming shopping malls into 21st century neighborhoods
As we reimagine the antiquated shopping mall, Marc Asnis, AICP, Associate, Perkins&Will, details four first steps to consider.