Daylight floods a comfortably furnished room where 10 patients sit in a circle, listening to an orientation by a registered nurse. Ranging from 40 years old to 70-something, all have Type 2 diabetes. Most of the 90-minute session will consist of a freewheeling discussion with an endocrinologist, encompassing symptoms, prognoses, prescriptions, and daily care. At the conclusion of the group meeting, a few patients will be examined in adjacent private rooms. Future sessions will involve a nutritionist, podiatrist, and ophthalmologist.
This is the so-called “shared medical appointment,” or SMA, and it’s a far cry from a standard 20-minute consult. The SMA epitomizes a new era in healthcare—one that views patients holistically rather than as an assortment of pathologies, and rewards providers for keeping people healthy. Though they’ve existed experimentally for more than a decade, SMAs are gaining traction for chronic conditions like hypertension, asthma, and celiac disease. Patients get extra time with the specialist, and the specialist makes more money, faster. (In the above scenario, the endocrinologist could bill insurers $100 an hour for each of 10 patients. Seeing them individually could take more than three hours.)
The traditional medical office building, designed to accommodate unrelated tenant groups in cookie-cutter suites, may be hard-pressed to accommodate emerging treatment models such as the SMA. Traditional MOBs typically lack appropriate spaces for affiliated, interdisciplinary physician groups, and they’re often inconvenient. Patients must travel to the MOB, which may be near a hospital but far from home, and then make further stops for imaging, lab work, therapy, or pharmacy services. Meanwhile, courtesy of the Affordable Care Act, healthcare systems are gearing up for a huge pool of newly insured patients, many of whom have relied on emergency rooms for primary care.
7 ways medical office buildings and outpatient facilities are changing
1. They reflect a shifting development model.
2. They’re more complex.
3. They’re more conveniently located.
4. They’re leaner.
5. They’re more digital.
6. They’re more aesthetically appealing.
7. They’re greener.
All these trends are forcing Building Teams and their clients to consider new styles of non-hospital facilities aimed at attracting patients, improving wellness, and saving money. Increasingly, healthcare organizations want to create “medical homes” that foster ongoing relationships and offer a competitive edge.
“Market analysis and community demand are factors that drive the services offered within an outpatient center,” says Brad Cardoso, AIA, Senior Healthcare Architect at Margulies Perruzzi Architects. “Often, care can be more efficiently provided by co-locating diagnostic services with primary care and specialty groups.”
Experts consulted for this article by Building Design+Construction all agreed that MOBs aren’t what they used to be. Here, in the second report in our series on Outpatient Facilities, are seven ways these buildings are changing in response to a new regulatory, economic, and technological environment.
1. The new medical office buildings reflect a shifting development model.
Not so long ago, developing an MOB was easy, says Patrick Fugeman, AIA, Director of Design & Construction for Delaware’s Christiana Care Health System. “Size it for maximum leasing flexibility, make it as long and tall as the site or pocketbook would allow, wrap it in a comfortable but not trendy façade, and sign up doctors and fit it out as discrete offices in a leased or condo arrangement.”
Today’s medical office is no longer just a real estate deal on or near a hospital campus, says Fugeman. “Rather, it’s an integral part of delivering a continuum of care, whether that’s a private development model or a partnership between a hospital and private practices.”
The Medical Office Building at the University of Kansas Medical Center, Kansas City, Kan., features six stories of outpatient clinics, consolidating previously discrete offices for more than 200 affiliated doctors. Clinical waiting rooms with flexible seating are arrayed along a meandering exterior wall, with semi-transparent panels separating transaction counters from the circulation path. To reinforce aesthetic quality, each floor houses an art gallery with seating and a vending area. Cannon Design and Turner Construction led the Building Team. PHOTO: GAYLE BABCOCK / ARCHITECTURAL IMAGEWORKS LLC
Teresa Wilson, a Principal at Steffian Bradley Architects , says traditional MOB design reflected a billing paradigm that still has an impact, in terms of federal requirements for reimbursement. “Facility licensing is not an issue if you’re only talking about tenant space with a lot of physicians who are not necessarily related and not giving a lot of support services. Today, though, the onus is on these organizations to provide wellness care, which creates a stronger incentive for putting the whole service component in one location.”
All of this is occurring in the context of the Affordable Care Act. In October 2012, the law started penalizing hospitals for high Medicare readmission rates. The ACA, rolling out in phases, also gives employers incentives for establishing wellness programs. The goal: keep patients out of hospitals, thereby reducing the alarming upward spiral in medical costs, which now account for 18% of the nation’s GDP—$2.7 trillion a year.
Hospitals are busily creating their own MOBs for groups of affiliated physicians, or are hiring developers to do it for them in leaseback arrangements. “Hospitals are buying space for longer terms, and they have better credit than individual practitioners,” says Sean P. McDonnell, Senior Director in Cushman & Wakefield’s Healthcare Practice Group. “They are renting for 15 to 20 years, and they have AAA credit, so they get much better terms and larger deals.”
Whatever the development mechanism, efficient delivery in a money-saving package is crucial. “There is intense pressure for hospitals and health systems to reduce the cost of providing care while simultaneously improving patient outcomes,” says Michael Petersen, AIA, LEED AP BD+C, EDAC, Director of Healthcare for Ware Malcomb.
2. The new medical office buildings are more complex.
Though the basic MOB, which offers simplicity and low cost, will still be around, owners are leaning toward buildings that are more flexible, collegial, and diverse. Floor plates are less boxy and are often larger, combining primary care, urgent care, specialty clinics, imaging, a lab, social services, a pharmacy, and sometimes even ambulatory surgery, all under one roof.
“We are finding that collaboration is paramount in delivering care to patients in a one-stop shopping area,” says Christiana Care’s Fugeman. “To do that, a larger footprint is preferred, with multiple interconnections and shared spaces.”
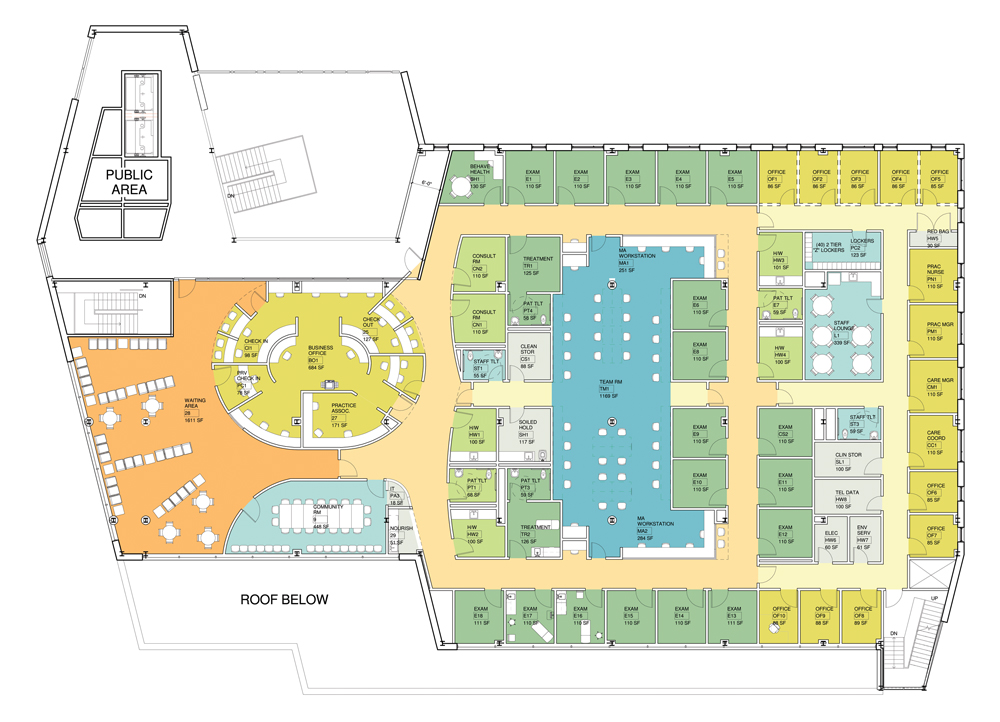
For Northern Edge Adult Medicine, a group of internists affiliated with Baystate Health in Springfield, Mass., Steffian Bradley Architects designed a facility where the usual array of exam rooms and offices is complemented by a large, open-concept team room (center, blue) and a community room (lower left, blue). Space for group work and shared medical appointments is increasingly important in outpatient care. PLAN: COURTESY STEFFIAN BRADLEY ARCHITECTS
As people live longer and their chronic conditions multiply, care will have to be better integrated, says Matt Richter, AIA, ACHA, Principal and Senior Architect/Planner at SmithGroupJJR. “Our aging demographic and a rising tide of complex co-morbid patient types will require more comprehensive team-based care, and outpatient facilities that can handle their demands efficiently.”
Catherine L. Gow, AIA, Principal of Health Facilities Planning at Francis Cauffman, says some of these facilities represent previously unthinkable hybrids. “Essentially, they’re hospitals without beds,” she says.
Gow cites Inova Health System’s Lorton Healthplex, one of many that Inova is locating throughout Virginia. Here, she says, patients find a freestanding emergency department, diagnostic imaging, a lab, an ambulatory surgery suite, and “a well-rounded balance of physician practice specialties to support the local community.”
The specialty-oriented facility, consolidating services for a single pathology or patient type, is another popular model. Kirsten Waltz, a Steffian Bradley Principal, points to Baystate Children’s Hospital Specialty Center, an outpatient pediatric site opening soon in Springfield, Mass. Divided into color-coded, easy-to-navigate neighborhoods, the building features a “playtrium” and a community room, handy for groups and family events.
“This is certainly more intense than an MOB,” says Waltz. “Cardiology, urology, pulmonology, gastro, endo—all these physicians will cycle through, and they’re all talking to each other. Care will be coordinated, so it is easier for patients to get answers. These are patients who are going to come frequently and have ongoing physician relationships.”
Even if a client asks for a fairly simple MOB program, it’s good to plan for potential complexity, says Brian B. Hirami, AIA, President of Stephen Rankin Associates (www.srankin.com). In particular, owners should consider the possible future need to accommodate an MRI suite, which would call for reinforced floors and an equipment access path through large, full-height windows. Hirami also recommends avoiding placing toilet rooms, which are expensive to relocate, along demising walls or in any zone where they might impede a reconfiguration or expansion.
3. The new medical office buildings are more conveniently located.
Providing a dazzling mix of services in the MOB is pointless if patients can’t get there, which isn’t always easy when diagnosis and treatment are hospital-based. That’s why healthcare organizations are fine-tuning their capital construction plans to make care more accessible to current and future patients.
“Doc-in-the-box and neighborhood clinic facilities are being strategically placed to capture patient load,” says Neil Humphrey, Senior Project Executive at Gilbane (www.gilbaneco.com). “Instead of a 30-mile drive to an acute-care hospital, these facilities will be in the mall down the street.”
Reliant Medical Group (an independent physician’s group) and Margulies Perruzzi Architects collaborated in an extensive lean design process for Reliant’s new Holden (Mass.) Family Practice site. The project consisted of a 17,700-sf tenant fitout within a 36,000-sf facility owned by healthcare provider Oriol Health Care. Reliant and the Building Team evaluated three exam-room mockups. Only high-scoring features were included in the final design, producing a standard to be used in all future Reliant clinics. PHOTO: WARREN PATTERSON PHOTOGRAPHY
Solutions range from walk-in clinics (often, in converted office, retail, industrial, or warehouse space) to purpose-built satellite health centers like Inova’s. “The centers are popping up everywhere,” says Cushman & Wakefield’s McDonnell. “Hospitals are trying to bring medical services closer to their key markets, in small locations, 5,000 to 10,000 sf, or buildings of 40,000 to 50,000 sf. It’s more of a retail experience. Ground floors and easy front access are important.”
Dan Perruzzi, AIA, LEED AP, Principal at Margulies Perruzzi Architects, cautions that even a pretty basic MOB may need a lot more power and HVAC infrastructure than a typical office, so selecting an appropriate reuse candidate may be tricky. “The capacity of the main electrical service and the distribution network should be carefully studied,” he warns. “The HVAC may not have ducted return air as required for medical uses. Patient access may require automatic sliding doors. Consider the route of travel for wheelchairs, walkers, and stretchers.”
Healthcare organizations are also relying on you to get facilities in place ahead of patient population growth. “Capturing market share means looking to AEC firms to help come up with innovative and speed-to-market solutions,” says Humphrey, “Many healthcare systems are now looking for fast-track construction and design-build alternatives.”
[PAGEBREAK]
4. The new medical office buildings are leaner.
The pervasive influence of “lean” thinking in medicine—to reduce waste, improve productivity, and achieve the best clinical outcomes—is flowing over to AEC firms, both in the buildings they create and in their delivery methods.
For instance, some outpatient facilities are providing the equivalent of a hoteling situation, with little or no private space for individual physicians, according to Steffian Bradley’s Wilson. “All the dollars are concentrated on the clinical space,” she says. “If the organization discovers that this is the most efficient use of doctors’ time, they can potentially see more patients and make more profit.”
Indicative of a growing focus on community-based care, the ACCESS Ashland Family Health Center serves Chicago’s South Side. ACCESS Community Health Network worked with RK Development, D+K Architects, and Fraton Construction on the 10,200-sf facility, which has 15 exam rooms, a living-room-like consultation space (also used for behavioral health), a lab, and an immunization room, plus a community room provided as a neighborhood service. Opaque architectural panels, alternating with IGUs treated with colored films, create a façade that balances the need for daylighting with privacy and security concerns. PHOTO: JACOB CLARY
Wilson says lean is part of the reason providers are starting to embrace shared medical appointments. Lean is also spawning models where patients stay in one space and specialists rotate to see them during a longer appointment, rather than making the patient bounce through multiple offices and facilities.
Another product of lean thinking is the facility template, whereby a healthcare organization crystallizes its best ideas in a design that can be replicated, customized, and scaled. SmithGroupJJR has created such a template for Phoenix-based Banner Health, with the group’s Maricopa, Ariz., clinic as the first built example. The prototype incorporates four basic models—Entry, Neighborhood, Community, and Regional—ranging from 18,000 to 105,000 sf.
“Templating is a highly iterative design approach and allows owners to build multiple facilities that are identical in planning concept yet adaptable to different locations,” says Lyle K. Steely IV, AIA, LEED AP BD+C, Associate and Design Architect at SmithGroupJJR. “It not only helps reduce the cost and time of design and construction, and thus speed to market, but also helps provide a universal standard of care among an organization’s facilities.”
5. The new medical office buildings are more digital.
While many physicians are struggling to master new electronic medical records systems, patients, too, will need to adapt to streamlined methods for organizing visits, with important implications for floor plans and communications infrastructure.
“Maximizing the available floor area for the patient/provider encounter means shrinking the spaces that don’t generate revenue,” says J. Andrew Jarvis, AIA, LEED AP, Healthcare Practice Director in EwingCole’s New York City office (ewingcole.com). “To reduce waiting room size, for example, we are now using new technologies such as self-service check-in kiosks, patient-location tracking systems, exam room occupancy sensors, and just-in-time scheduling to reduce or eliminate the wait. These strategies not only save floor area but also improve patient satisfaction.”
Providers that offer shared medical appointments need rich A/V technology so off-site specialists can be part of the session mix, says Margulies Perruzzi’s Cardoso. Ware Malcomb’s Petersen predicts that telepresence, cloud computing, and artificial intelligence will eventually revolutionize care—reshaping buildings and eliminating some site visits altogether.
Steffian Bradley’s Waltz agrees. “You won’t need so much parking. You won’t need registration. It could end up being simple as Skype with your physician. The problem is the billing and reimbursement catching up. But I think it’s definitely coming.”
6. The new medical office buildings are more aesthetically appealing.
In their fight for market share, healthcare providers are striving to improve the stereotypical image of the MOB. “The competitive environment has fueled the already popular patient- and family-friendly feel that clients are striving for,” says Francis Cauffman’s Gow. “Consumerism is king,” she says, and with women making most healthcare decisions for the family, institutions are choosing materials and finishes that create a spa- or hotel-like feel.
Jason Harper, AIA, LEED AP, Associate Principal, Healthcare, at Perkins+Will New York (www.perkinswill.com), says the Affordable Care Act will give many patients new healthcare choices, and providers want to make sure their facilities are a long-term draw. “Healthcare is increasingly being delivered in branded, retail-like outpatient centers that are geared toward a relatively fickle customer who needs ongoing care due to one or more chronic conditions.”
The desire to create a pleasant facility, as well as an effective one, is evident in Kaiser Permanente’s Antelope Valley Medical Offices, under construction in Lancaster, Calif. With a Building Team including architect/interior designer TAYLOR and contractor McCarthy Building Companies, the facility encompasses 137,000 sf, including 94 exam rooms and offices for 66 specialty physicians. Indoor and outdoor common spaces, a healing garden, and amenities such as an open-concept café are intended to serve both staff and patients. Poppies and butterflies, native to the mountain locale, are a prominent design theme.
Some adaptive-reuse jobs, such as the 55,000-sf outpatient center that Environetics recently created for Lourdes Health System in Cherry Hill, N.J., also reflect owners’ concern for curb appeal. Built in a former supermarket, the LourdesCare site features an expansive glass storefront, offering views into nicely furnished spaces combining wood and natural stone walls.
7. The new medical office buildings are greener.
Concerns about sustainability and life cycle costs have been extended from the hospital to the outpatient facility, especially as primary care moves from low-tech office environments to more resource-intensive buildings.
“The greening of MOBs is a trend, with requirements for new items from bike lockers, showers, and electric-vehicle charging stations to super-efficient HVAC systems to reduce energy consumption,” says Bill Foulkes, Vice President and Regional Manager with healthcare consultant Hammes Company (www.hammesco.com).
ColumbiaDoctors Midtown, designed by Perkins+Will for Columbia University Medical Center, is a new outpatient facility in central Manhattan, supporting 225 doctors, dentists, and nurse practitioners. Designed to draw urban professionals, the project, which renovated an existing nonmedical office building (in itself a highly sustainable strategy), achieved LEED Gold. Kaiser Permanente’s Antelope Valley building is shooting for both net-zero and LEED Platinum.
Reducing travel—and, presumably, greenhouse gas emissions—is a less heralded but potentially significant sustainability benefit of placing healthcare facilities closer to patients’ homes and workplaces.
There’s plenty of debate about the best ways to deliver outpatient services in a brave new regulatory world. But experts all agree on one point: the MOB will change. To remain competitive, Building Teams will need to do deep research on healthcare trends, and engage in frank discussions with their clients.
“It is paramount that we understand our clients’ business models so we can successfully design and build facilities that serve their needs and fit their brand,” says Angeles Garcia-Tapia, Project Director, McCarthy Building Companies (www.mccarthy.com). “Healthcare demand, cost, and efficiencies are going to drive the new standard of services for MOB construction and renovation.”
Related Stories
Legislation | Mar 21, 2024
Bill would mandate solar panels on public buildings in New York City
A recently introduced bill in the New York City Council would mandate solar panel installations on the roofs of all city-owned buildings. The legislation would require 100 MW of solar photovoltaic systems be installed on public buildings by the end of 2025.
Products and Materials | Feb 29, 2024
Top building products for February 2024
BD+C Editors break down February's top 15 building products, from custom-engineered glass bridges to washroom accessories.
Modular Building | Feb 6, 2024
Modular fire station allows for possible future reconfigurations
A fire station in Southern California leveraged prefab, modular construction for faster completion and future reconfiguration.
Government Buildings | Jan 29, 2024
Army Corps of Engineers moves into new engineering and support center
The building, in Huntsville, Ala., combines office and warehouse spaces.
Sponsored | BD+C University Course | Jan 17, 2024
Waterproofing deep foundations for new construction
This continuing education course, by Walter P Moore's Amos Chan, P.E., BECxP, CxA+BE, covers design considerations for below-grade waterproofing for new construction, the types of below-grade systems available, and specific concerns associated with waterproofing deep foundations.
Museums | Jan 8, 2024
Achieving an ideal visitor experience with the ADROIT approach
Alan Reed, FAIA, LEED AP, shares his strategy for crafting logical, significant visitor experiences: The ADROIT approach.
Government Buildings | Dec 19, 2023
New Pennsylvania State Archives building holds documents dating back to 1680
Work was recently completed on a new Pennsylvania State Archives building in Harrisburg, Penn. The HGA-designed, 146,000-sf facility offers numerous amenities, including computers, scanners, printers, a kitchenette with seating, lockers, a meeting room, a classroom, an interactive video wall, gallery, and all-gender restrooms. The features are all intended to provide a welcoming and comfortable environment for visitors.
Giants 400 | Dec 12, 2023
Top 15 Veterans Affairs Facility Construction Firms for 2023
Walsh Group, Turner Construction, BL Harbert, and Hoar Construction top BD+C's ranking of the nation's largest Veterans Affairs facility general contractors and construction management (CM) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report.
Giants 400 | Dec 12, 2023
Top 20 Veterans Affairs Facility Engineering Firms for 2023
IMEG, Specialized Engineering Solutions, KPFF Consulting Engineers, and Heapy head BD+C's ranking of the nation's largest Veterans Affairs facility engineering and engineering/architecture (EA) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report.
Giants 400 | Dec 12, 2023
Top 35 Veterans Affairs Facility Architecture Firms for 2023
LEO A DALY, Page Southerland Page, Guidon, and HDR top BD+C's ranking of the nation's largest Veterans Affairs facility architecture and architecture/engineering (AE) firms for 2023, as reported in Building Design+Construction's 2023 Giants 400 Report.