Creating a home for eldercare using the ‘Green House’ design concept
The U.S. population is aging. In 2050, Americans aged 65 will number 83.7 million, almost double the elderly population in 2012. The baby boomer generation seeks a more dignified and affirming experience for its later years. The institutional feel of the “nursing home” our parents or grandparents may have spent time in is no longer considered acceptable. To respond to this aging population, the design for eldercare facilities must become increasingly compelling. Various eldercare design concepts have emerged over the past fifteen years, all providing an alternative to the institutional-type residential care setting for those seeking them, either by convenience or necessity.
The Green House is one promising concept. Founder Dr. Bill Thomas revolutionized the care of elders with the Eden Alternative, a non-profit network of communities dedicated to quality of life for seniors, from which the Green House Project evolved. The Green House is a “home-like residential care facility comprised of 10 to 12 single occupied units with full baths and all common areas to accommodate residents in a comfortable, homelike environment.”
The Green House is a home-like residential care facility comprised of 10 to 12 single occupied units with full baths and all common areas to accommodate residents in a comfortable, homelike environment.
The Green House small-house model of long-term care emphasizes the vitality, autonomy and dignity of elderly residents. Its founders and proponents believe this new model must be accompanied by cultural change which supports the privacy and security of the residents, gives them meaningful activities and allows them to function to the best of their ability.
The Green House concept works for a wide range of patients including those requiring special geriatric care, memory care and severe head trauma care. It is an especially effective environment for individuals with cognitive impairment. Persons with dementia or cognitive disabilities are better served in this very personal and open medical home model. The flexibility and tolerance of this model accommodates an assisted living population with diverse needs.
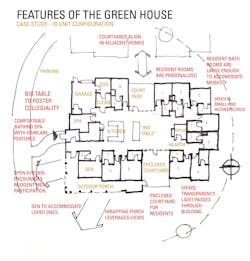
After a recent visit to the Milwaukee VA Medical Center’s Green House Green House Community Living Center, the VOA team reflected on how we would envision implementing the Green House concept into our future eldercare project designs. The following design considerations are key aspects of the Green House:
Planning: Is the Green House located on a larger campus, or is it set apart? How are groupings of houses arranged, where will parking for staff, visitors and service personnel be located? Will each CCRC (continuing care retirement community) be designed separately? Can a project budget for infrastructure separately from the CCRCs? Green House community living centers tend to be either be arranged in a loose cluster along a ring road or more strictly arranged to create more formal and contained outdoor spaces.
Square footage: How big is the facility? Green Houses, designed for 12 or fewer residents, can be constructed with around 8700 SF of interior space.
Operational connection to the larger medical center: How are operations related to a larger medical center? Operationally, the Green House assumes there will be three FTEs (two universal care staff, and one RN) to support the facility, meaning residents only need to know three team member names – further promoting the feeling of “family” and “home.”
Certified Nursing Assistants are trained in everything from food preparation to care and patient opportunity with attention to dementia care. Clinical support team (physicians, nurses, therapists and other professionals) visit the site as needed. The Green House is autonomous except in regards to groceries, waste/garbage pickup, and pharmacy/medication needs.
Promotion of Social Interaction: How does the Green House concept promote social interaction in the eldercare setting? The Green House features larger open spaces including a large living room for gathering, a central kitchen and a smaller “den” for smaller group gatherings and entertainment in a more intimate setting (card playing, movie watching, etc.) A large dining table is prominently featured in the large open gathering are to promote the feeling of being at home and part of a larger group.
Personalization: At the VA Green House, one’s own furniture can be used in a bedroom, and residents bring in their own refrigerators, musical instruments and so forth—personalizing the spaces and adding to an overall homelike feel.
Steps to De-institutionalize: In creating the residential feel, the Green House concept also does away with the nurse station and other institutional needs such as carts and PA systems. A Green House has a small office (approximately 120 SF) where all of the back of house paperwork, office needs are taken care of.
Programmatic Considerations: Lastly, the Green House concept employs design strategies to maintain the residential scale.
Scale: Does the home feel like a “home” in scale, and if so, how so? The Green House facilities are frequently designed and detailed with a residential feel that speaks to the local context. The residential feel is mainly felt in the larger living room and the dining area, while the patient rooms and others support spaces are more utilitarian.
Residential pattern: The Green House has a residential pattern to it to allow the rhythm of life to play out in its spaces. The residents should feel at home there. This residential quality permeates the interior spaces and the adjacent exterior spaces – including enclosed patio/porch and contained outdoor spaces which promote interaction with nature and exposure to natural light.
Programmatic spaces: Our sketch above depicts the spatial relationships and communal elements comprising the program for an elder care facility that embraces the Green House concept.
For more information or to tour Green House Projects, visit thegreenhouseproject.org.
About the Author: Douglas J. King, AIA, NCARB, CSI, ACHA, is an instrumental leader in VOA’s Healthcare practice, with a particular emphasis on VOA Federal Healthcare. He is an active and visible voice in his industry, with presentations that span the globe and articles published in Facility Care Magazine and Matrix Magazine, among other publications. As a code and regulatory expert, Doug has served on several committees for the Illinois Department of Public Health, and is part of the AIA sub-committee for preparing national standards. Doug also supports the education and mentorship of young architects, serving on advisory committees for two architecture schools that offer Masters concentrations in Healthcare Design.
About the Author
Stantec
Published by global design firm Stantec, this eclectic blog features viewpoints, insights, and explanations from Stantec architects, engineers, and designers, on a range of issues impacting the fabric of our communities. Our contributors share their thoughts about design trends, emerging technologies, vexing challenges, and inspired solutions. For more blog posts, visit our Ideas page. Follow us on Facebook, Instagram, LinkedIn, and Twitter, and YouTube.