Easing the oncology journey: The role of urgent care
Cancer treatment is not a smooth road. Patients react to drugs and treatments differently, encountering a myriad of side effects. When oncology patients experience these sometimes alarming side effects or complications, the options for immediate medical care are often limited and are not the best fit for them. Outpatient cancer centers are not open 24/7, but many complications can’t wait until the next day. As a result, many oncology patients turn to the emergency department (ED), sometimes leading to inpatient admission. Unfortunately, both of these environments increase the risk for immunocompromised patients by exposing them to pathogens while they wait for treatment.
Oncology patients are better served when they’re connected to the right staff. Emergency physicians are typically not cancer experts and are not familiar with an oncology patient’s history, longitudinal care plan, and drug therapy the way their cancer team is. Because of this, they are less able to rule out other causes of the symptoms presented. This results in unnecessary tests and longer stays – all while patients continue to suffer symptoms and remain exposed to health risks in an ED or inpatient setting.
There is a better way. An oncology urgent care model can keep patients within your system, with doctors and a care team who know their case. Clinicians who understand the side effects and interrelated issues that arise from longitudinal cancer treatments can move straight to the remedy. All of this can be done while keeping your patients in a more comfortable and controlled environment that is less variable than an ED waiting room or bay. In what follows, we explore operational strategies necessary for effective oncology urgent care and provide recommendations to help health systems to determine and implement the right oncology urgent care strategy for them.
It is our hope that oncology urgent care can be more widely adopted to elevate the patient’s treatment experience while decreasing unnecessary suffering and improving clinical outcomes.
MAXIMIZE AGILITY & ACCESS
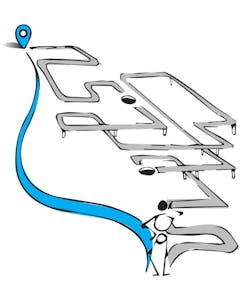
While the prospect of offering urgent care services to their patients is intriguing, many oncology programs often get stuck on how to operationalize the idea. Should they dedicate space within their program or partner with the ED? How should they staff the program? With what clinicians? Instead of thinking about this service line as a self-contained “box,” we recommend thinking about it as a portal within which an oncology patient can receive a spectrum of care, including a safer, more comforting place to triage and wait if emergent care or hospitalization is needed. An important plank in your platform of comprehensive care, oncology urgent care promises to improve patient experience and provide a strong market differentiator.
Keep in mind that urgent care can take many forms:
- Virtual Care (telehealth and the evolving remote patient monitoring platforms) would provide access to clinicians who can discuss symptoms and provide feedback on how to manage symptoms from home, when to seek in-person help, and prescribe additional medication if needed. This kind of check-in helps ensure proper, timely care and leads to improved compliance with medication. While improving patient care now, this platform will also lay the foundation for the eventual influx of data from ongoing remote patient monitoring applications, leading to future innovations.
- Patient Segmentation within the systemwide ED would allow oncology patients to be fast-tracked into a separate care pathway following an urgent care referral, where a staff oncologist can better target what’s causing distress and get to treatment sooner.
- Hybrid Care is also an option. For example, infusion centers tend to be open extended hours and an exam room plus a reserved infusion bay or two may allow a version of urgent care to be incorporated within this department. Flexible exam rooms can be converted into secondary uses like waiting, infusion or consultation.
- Palliative Care should be integrated into any oncology urgent care platform. Helping oncology patients manage their pain is an urgent need and an immensely valuable oncology service.
- Home-Care and Home-Infusions are growing in demand. As this growth continues, it’s important to keep your oncology patients connected to your system for better longitudinal care. Having access to an ad-hoc urgent care visit gives patients the security of knowing that their oncology team and physician can be accessed immediately through the urgent care model
UNDERSTAND YOUR CARE MODEL
Simply launching a program isn’t a recipe for success. It’s important to have a comprehensive and integrated strategy that leverages the resources of the entire health system. If you have a sufficient volume of oncology patients to develop a dedicated Urgent Care Center (UCC), you may want to consider strategies for a gradual implementation in order to defray costs. For example, due to physical or financial constraints, your system might not be ready for a full-service oncology UCC today. But by building shared, multipurpose space, you can offer the desired service and grow strategically into your oncology urgent care program. You could also hybridize your solution, incorporating oncology-adjacent programs that have natural partnerships and concentrate expertise. Consider a phased pathway based on program maturity.
For example:
Phase 1: Oncology & Palliative Care UCC
This would address the needs of current patients in your system’s cancer services by providing access to a medical oncologist practitioner in an urgent care setting along with access to a palliative care expert. Complications from cancer treatment often require and benefit from palliative intervention.
Phase 2: Oncology & Survivorship UCC
Once the UCC is capable of effectively managing the flow of patients who are in active treatment, this phase might involve extending urgent care services to survivors. Given their individual medical histories and responses to cancer, this population is unique and would benefit from oncology-centric thinking and longitudinal medical teams.
Phase 3: Oncology & Cardio-Oncology UCC
Cancer and its treatments affect other parts of the body as well. Leveraging a health system’s full care portfolio in order to integrate other specialties such as cardiac care or internal medicine into cancer care provides an advanced phase of urgent care while simultaneously expanding the survivorship umbrella.
An oncology UCC is different than a traditional UCC. Its drivers can be tuned to help your oncology service save money and resources by putting the patient at the appropriate level of care needed for their requests; improve patient satisfaction; and reduce clinical complications. By studying several successful UCC models across the nation, we can also recommend some best practices for operations:
- Consider screening patients prior to making an UCC appointment to determine if the patient navigation is more appropriate for a telehealth visit or referral to the UCC.
- Have a strategic growth plan to help determine what you require in a UCC program. This will also help you to determine critical adjacencies to departments like pharmacy, labs, imaging, and procedure teams.
MAKING IT WORK FOR PATIENTS
It’s important to understand your risks and patient population to develop a targeted strategy. We like to think about it as a triple-win opportunity. First, depending on how you view your service line vs. your system’s finances, an oncology UCC can reduce overall cost to the system for an oncology patient while simultaneously improving clinical outcomes, and increasing patient satisfaction. Second, it reduces inefficiencies in the ED and inappropriate admissions to your inpatient service. Third, immunocompromised oncology patients have a reduced chance for acquiring an infection or illness by waiting and receiving treatment in a non-specialized UCC, ED, or inpatient facility.
As a key support during a very sensitive time, an oncology UCC tells your patients and their caregivers that you care about their experience, their health, and their caregivers, and that you’ll be there when they need you.
About the Author
GBBN
We combine creative tenacity, technical mastery, and a global perspective to deliver design solutions that help our clients achieve their goals. Together, we shorten the distance between medical breakthroughs and patient bedsides, set students up for success, connect audiences and artists, and inspire employees to do their best work. At GBBN, we see architecture as mor than just buildings, because positively affecting people is the most important thing we do. Follow GBBN on Facebook, Instagram, LinkedIn, and Twitter.