Planning, designing, financing, and constructing healthcare projects has never been more onerous for hospital administrators and boards. Capital dollars are scarcer than ever, and reimbursements from Medicare, Medicaid, and private insurers are getting squeezed. In such an environment, capital projects had better come in under budget and ahead of schedule to get badly needed revenue streams flowing.
“It’s all about providing the highest value at the lowest cost,” says Philip Tobey, FAIA, FACHA, senior vice president at SmithGroupJJR and an editorial advisor to this publication.
Overshadowing all this is the Patient Protection and Affordable Care Act of 2010—or, as its detractors call it, Obamacare. For hospital administrators, the healthcare law is something of a black hole. Will new federal regulations kick in as planned in 2014? How would a Republican victory in the upcoming election affect the law? What level of reimbursement can hospitals expect to receive under the new law? Will payments be pegged to better patient outcomes?
Throw in the unknown effect of new technologies, protocols, and procedures, and it’s easy to see why the nation’s hospital systems are desperate for ways to save money while trying valiantly to maintain quality.
Such a climate of uncertainty “forces decision makers to predict a future state that is inherently unpredictable,” says David Watkins, FAIA, chair and founding principal of WHR Architects, Houston.
Fortunately, the AEC industry has developed new tools and techniques to ease the burden on beleaguered healthcare administrators. Let’s take a look at these strategies.
1. Move less critical functions to lower-cost space
Main lobby at Beatrice (Neb.) Community Hospital. Less intense spaces like this were serviced with ductless plenum air returns and lower-cost fire-suppression equipment, which helped bring construction costs down to $223/sf, according to Loren Lamprecht, AIA, president of Altus Architectural Studios.
Many 20- or 30-year-old facilities are short on the latest technology and long on high-cost inpatient bed capacity. “Healthcare systems are building more integrated care spaces, combining, say, outpatient surgery and chronic disease management,” says Patrick Duke, senior vice president with KLMK Group, a Richmond, Va., firm that advises healthcare systems on capital planning. Instead of locating such facilities in an expensive downtown campus, they often wind up in a lower-cost suburban strip mall—in what Duke calls “a nice 30-year building, instead of a 50-year monument.”
Methodist Hospital System, in Houston, has put a planned expansion of its downtown space on hold, even as it has been pursuing a suburban expansion strategy in recent years. “Methodist decided that they need to live within the buildings they have for the next five to eight years,” says Watkins. By consolidating functions, reallocating space more efficiently, and making use of unused shell space, the hospital will wring as much use out of its current footprint as possible.
WHR is advising Methodist management on which departments, if any, can be moved or consolidated. Not every option will turn out to be feasible. “We may end up with areas that cannot move because of scheduling and cost issues,” says Watkins. “Sometimes the disruption and lost revenue from a move are not worth it.”
Some greenfield projects and expansions create lower-cost space within the same building. The recently opened Beatrice Community Hospital in Beatrice, Neb. (2009 population: 12,564) is divided between an institutional zone—for inpatient, intensive care, and diagnostic services—and lower-cost space for administrative, lab, physical therapy, dining, pharmacy, and other less intense functions.
Omaha-based Altus Architectural Studios designed the 144,000-sf facility to save money by equipping the institutional zone with ducted air returns to each room and a high fire rating, while the low-intensity zone has plenum air returns (no ducts required) from the drop ceiling and lower-cost fire-suppression features. “Mechanical systems typically make up 45-50% of the cost of such a building,” making them a high opportunity area for savings, says Loren Lamprecht, AIA, NCARB, Altus’s president. Altus was able to bring in the project’s construction cost at $223/sf, compared to a similar project in Nebraska that came in at $268/sf—a 17% difference.
[pagebreak]
2. Design spaces to increase patient throughput and staff efficiency
Twenty-nine bay observation unit at Detroit Medical Center, a renovation of a 5,800-sf physiotherapy space. A customized headwall design using a modular, prefabricated solution with pre-installed medical gasses works anywhere in the space.
A renovation that created a short-term observation unit at Detroit Medical Center highlights another cost-saving trend. The 29-bed, 5,800-sf unit provides space for patients referred from the ER at Detroit Receiving Hospital, one of nine hospitals in the Detroit Medical Center. The center’s ER traffic has increased more than 60% in the last decade, from 68,000 patient visits in 2001 to 110,000 in 2011, according to Ruth Kremer, the DMC’s communications director.
The revamped space, previously dedicated to physical therapy, accommodates non-acute patients who need less than 24 hours of monitoring. The unit is staffed by nurse practitioners and skilled nurses; staff physicians make rounds and are on call, but are not assigned full time to the unit.
The new staffing strategy was prompted by changes in reimbursement. “Insurers are reimbursing [only] nominally for patients that just receive observation,” says Kremer. The new space is helping the hospital implement a lower-cost staffing solution for an increasingly costly function.
Another way to save money on space is to build less of it. Recent healthcare designs have pared back square footage on lobbies, dining areas, and other nonclinical functions. At Presbyterian Hospital, a new facility in Flower Mound, Texas, HKS Architects steered away from an expansive lobby and created a courtyard off a relatively modest lobby. “The courtyard is less expensive to maintain than an indoor area.” says Shannon Kraus, AIA, ACHA, LEED AP, an associate principal and senior vice president at HKS.
Scaling back nonessential space not only saves on initial costs, but also on long-term maintenance. According to healthcare consulting firm Kaufman Hall, each square foot of space costs $30-40 a year to heat, cool, insure, clean, and refurbish over a hospital’s lifetime.
Designs that allow healthcare facilities to operate more efficiently after the ribbon cutting can add significantly to value. At the new 286-bed Middle Tennessee Medical Center in Murfreesboro, Gresham, Smith and Partners laid out each floor on a 72-bed chassis, broken into four 18-bed pods that operate independently. “No patient room is more than 75 feet from a nursing station,” says Greg Gore, AIA, NCARB, Gresham’s principal-in-charge. This contrasts with traditional designs that had some patient rooms as far as 200 feet from a nursing station. Cutting down on unnecessary walking gives nurses more time to care for patients.
[pagebreak]
3. Apply Lean principles and integrated project delivery

Patient room at Mercy Medical Center Merced. Using Lean principles, the IPD-based Building Team of RBB Architects and McCarthy Construction Cos. saved the owner $3,725,000 in structural construction costs and $542,000 in MEP costs on the eight-story acute care tower. The team even helped the hospital pick up a $120,000 rebate from the local irrigation district.
Lean principles, as espoused by the Lean Construction Institute (www.leanconstruction.org), probably have their greatest following in the healthcare sector. Nearly half (47%) of architects responding to a survey of attendees at last fall’s Health Design Conference agreed that “Lean practices, where teams analyze processes and improve operational efficiencies before designing a new facility,” will be prevalent over the next couple of years. Fifty-four percent of healthcare providers said preference for IPD is growing; 83% of architects agreed.
The case of Mercy Medical Center Merced, a 196-bed replacement hospital in Merced, Calif., underscores the potential of Lean and IPD in controlling construction costs while meeting client demands for high-quality design.
When Mercy’s parent firm, Catholic Healthcare West (now Dignity Health), decided to consolidate two existing campuses into one facility, it called upon RBB Architects (designer), McCarthy Building Cos. (GC), and Harris & Associates (PM-CM) to manage the project using Lean, IPD, and a hybrid form of design-assist with the California Office of Statewide Health Planning and Development (OSHPD).
The Building Team took a year and a half just in pre-planning and preconstruction.
Strict protocols were put in place to guide construction delivery. Schedule revisions had to be signed off by all subcontractors and the client. Weekly progress meetings, chaired by McCarthy, used short interval scheduling to monitor and control short-term site activities.
The firms had to commit to hands-on participation by their principals. The client required continuity of the design-assist team leaders who were working with OSHPD.
The 267,000-sf acute care facility opened in 2010 at a construction cost of $167 million and total project cost of $248 million. Patient room size was capped at 1,400 sf, compared to an industry average of 2,150 sf, according to RBB Architects. Construction cost per bed was held to $850,000, vs. an average $1.4 million per bed for the region—a savings of 30%. Change orders were kept to less than 1%. Incremental permitting enabled construction to get started a year early; the project was delivered 60 days ahead of schedule.
As part of the IPD agreement, the Building Team is currently conducting a four-phase post-occupancy evaluation, which has already unearthed a few problems. Hospital staff complained that the storage space in patient rooms was too small. An upholstery fabric was found to be less stain resistant than anticipated. Manual shades in patient rooms were noisy and hard to operate; the Building Team vowed to “advocate more fiercely” for motorized shades in future projects.
Considering the size and complexity of the project, these problems seem relatively minor.
[pagebreak]
4. Make spaces more flexible for multiple uses

Stamford (Conn.) Medical Center, designed by WHR Architects. The facility’s emergency department will link triage and testing/treatment rooms to move less critical patients more quickly through the ED. This will enable staff to provide a quick evaluation and appropriate level of care.
Making space as flexible as possible so that it can accommodate a variety of functions or be repurposed in the future at reasonable cost is an increasingly popular highest-value trend. In a survey of attendees at last fall’s Healthcare Design Conference, Mortenson Construction found that nearly half (48%) of healthcare provider respondents “strongly agreed” that healthcare designs must put greater weight on flexibility to address uncertainties in markets, care delivery, and patient volume.
To save money for Middle Tennessee Medical Center, Gresham, Smith and Partners took two departments that traditionally have been kept apart—preadmission testing and the ER—and put them back-to-back.
“The ER tends to be busiest in the evening, while the preadmission area is busiest during the day. We put them back to back so that they would provide surge capacity for each other,” says Gresham’s Gore. Each area has 10 equally sized rooms containing the exact same equipment, thus enabling staff to provide either ER care or preadmission testing in either space.
Stamford (Conn.) Medical Center, designed by WHR, employs a similar ER strategy. “If the staff need to do a test like an EKG, there’s a testing room behind the triage space,” says Charles Cadenhead, FAIA, FACHA, FCCCM, a senior principal with WHR. “The goal is to give a quick assessment and the most appropriate treatment as fast as possible.”
The linkage of triage and testing/treatment rooms speeds up this process. Triage takes about 15 minutes per patient, and about 10% of patients are released right after being examined. Under the old protocol, all patients would be sent from triage to an examination room to wait for a physician’s evaluation. Now, the staff can triage and diagnose in the same room, allowing them to treat more patients in a given time period, thereby increasing patient throughput.
[pagebreak]
5. Use prefabrication to trim construction costs, shorten schedule

A unitized curtain wall being fabricated at a remote site for Lakeway (Texas) Medical Center. Hoar Construction used these prefabricated systems, along with prefab overhead piping and ductwork, to lower costs and speed delivery of the project, which came in two months ahead of schedule.
Building Teams are using factory-based prefabrication to save time and money—and improve quality of workmanship—in hospital projects, especially in cases where repetitive design elements come into play.
For the Lakeway (Texas) Medical Center, Hoar Construction used prefabricated elements—a unitized curtain wall on the east end of the building, and overhead piping and ductwork—that were manufactured offsite in a controlled environment. The process helped shave two months off the construction schedule. “That’s two more months for the hospital to make revenue,” says Michael Booth, Hoar senior project manager.
The unitized glass curtain wall was tested for leaks before it left the factory, saving time and headaches on the job site. “You don’t have to deal with the elements and worry that you have the right caulk to create a good seal in the joints,” says Booth.
Precast concrete fabricated offsite saved time and money on the new Methodist Women’s Hospital and Medical Office Building in Omaha. HDR Architecture, Inc., used thin-brick-embedded precast concrete construction to simulate a brick-and-limestone façade. The 116-bed facility and a companion medical office building are highly visible to the neighboring upscale suburban community, so aesthetics were important to the client—but so was saving money.
Using the thin-brick precast system trimmed the amount of raw material required from 999 tons to 178, according to the fabricator, Endicott Clay Products, Fairbury, Neb. Of course, that also saved on delivery costs. For this strategy to work, however, the prefabricator has to be located within reasonable shipping distance from the construction site, warns Brian Halsey, AIA, LEED BD+C, an associate vice president with HDR. “You also need a crane for installation, so ideally you want to be able to get one located fairly close by,” he adds.
As Building Teams become more familiar with prefab options, manufactured systems will continue to find their way into healthcare projects.
[pagebreak]
6. Look into performance contracting for energy-efficiency
Musgrove Park Hospital, a World War II-era public hospital, will save $1.1 million a year in energy costs over 12 years through retrofits made under a performance contract with Schneider Electric.
Rising energy costs are of increasing concern to hospital administrators. While energy expenses are not a huge percentage of operating budgets, new energy-efficiency options offer more ways to trim utility bills—savings that will only get better as utility costs go up. And because capital investment funds are hard to come by, performance contracting has become a more viable means to upgrade systems without a capital outlay.
Healthcare Providers Agree: DESIGN COUNTS
Improving facilities and their physical design substantially:
- Improves patient experience 74%
- Improves staff effectiveness 60%
- Improves staff recruiting/retention 59%
- Improves patient outcomes 57%
- Attracts new patients 54%
Nearly three-fourths (74%) of healthcare providers surveyed by Mortenson Construction agreed that improving facilities and their physical design “substantially” improves patients’ hospital experience. Source: Mortenson Construction, “Healthcare Industry and Facility Design Trends,” January 2012
In the United Kingdom, Musgrove Park Hospital, a World War II-era public hospital in Taunton, Somerset, is in the midst of a massive upgrade of its steam, hot water, heating, and lighting systems. Acting under a performance contract with the hospital, Schneider Electric is implementing technologies such as combined heat and power, automated lighting, and HVAC controls that power down fans when a space is unoccupied.
Funded with private capital, the agreement guarantees about $1.1 million in annual energy savings over 12 years. Schneider is paid back from the savings on utilities. If the improvements fail to reduce energy consumption by the amount stated in the contract, Schneider must make up the difference, according to Simon Rigby, divisional director, clinical support at Taunton and Somerset NHS Foundation Trust. The initiative is also projected to slash the facility’s carbon emissions by 43%, which is significant because hospitals in the U.K. are under mandate to reduce greenhouse gas emissions 34% by 2020, and 80% by 2050.
According to Schneider Electric’s Tammy Fulop, performance contracting is starting to make inroads in the U.S. healthcare sector. “It’s not as far along as it is in the university and government sectors,” she says, but it is starting to attract interest in hospital C suites.
[pagebreak]
7. Help clients develop firm standards for construction project
Combined with patient safety and quality of care, cutting costs and adding value are top-of-mind concerns for Building Teams serving the vital and lucrative healthcare sector.
From its base outside St. Louis, Mo., Ascension Health, a ministry of the Daughters of Charity and Sisters of St. Joseph, operates 80 acute care facilities nationwide. To lower project costs and add to design value, Ascension’s five-member facilities planning staff, four design firms, several GCs, healthcare professionals, and others spent 15 months devising a 100-page guide for new construction and renovations covering standards for room size, overall square footage, mechanical and electrical infrastructure, and numerous other building features. The standards are aimed at cutting first costs, with high priority placed on energy savings, but exceptions can be made when spending more up front would yield lower total cost of ownership.
All projects of $10 million or more must comply with these standards and be approved by the facilities planning department, headed by Bob McCoole, vice president of the facilities resource group. McCoole says there has been some pushback at the local level: “Some projects have come in with a number of exception requests,” many of them of the “that’s-the-way-we’ve-always-done-it” variety. McCoole says his job is to determine whether an exception would improve the quality of care or service, or make the facility more efficient. A request for a three-story water feature isn’t going to get very far.
The good news is that healthcare construction, while off slightly from more halcyon days, remains quite solid. Three of four respondents (75%) to the Mortenson survey said their institutions’ construction activity would be at least “moderately greater” in the next 12-24 months—with 27% saying it would be “substantially greater.”
However, given current economic straits, hospital systems can no longer afford to build the kinds of elaborate monuments that, in decades past, could be justified on the basis of providing a marketing edge. That’s not to say that the next generation of hospitals should look cheap, drab, or utilitarian. But, along with assuring patient safety and quality of care, cutting costs and adding value have got to be top-of-mind concerns for Building Teams serving this vital—and still lucrative—sector. +
[pagebreak]
Princeton Healthcare System: Applying the '70/30 rule'

Princeton HealthCare System’s University Medical Center at Plainsboro, designed by HOK (with RMJM Hillier), with Syska Hennessy as MEP engineer, Turner Construction as GC and Navigant as PM/development adviser. It opens May 22.
The 231-bed replacement hospital that Princeton HealthCare System (PHCS) is about to open in Plainsboro, N.J., is based on an intense reorganization strategy developed through something called the 70/30 rule.
“The 70/30 rule says that 70% of organizational improvement comes from re-engineering your existing operations. The other 30% comes from the physical design,” says the rule’s progenitor, Fred Campobasso, managing director for healthcare at Navigant, PHCS’s development adviser and program manager.
Barry Rabner, PHCS’s CEO for the last decade, and his board brought in the consultant several years ago, when it became clear that the 93-year-old hospital in downtown Princeton needed to rethink its entire organization in order to compete with local rivals Capital Health Regional Medical Center, in Trenton, and Robert Wood Johnson University Hospital, in New Brunswick—not to mention quaternary hospitals less than two hours away in Philadelphia and New York.
With Navigant’s counsel, PHCS officials engaged in a robust strategic planning process that included tours of a dozen other hospitals. From this came a set of guiding principles—notably, to reduce infection, errors, falls, and operating costs, and to improve clinical outcomes and patient satisfaction.
These are fairly common guidelines, but PHCS planners took them very much to heart. “Every time we had a decision to make, we would look at the guiding principles,” says Rabner.
The key question: whether to rebuild in downtown Princeton, or move out altogether. “Our patient population was growing, but 70% of our market was coming from the region, not from downtown,” says Rabner.
Navigant helped the PHCS staff evaluate 10 core processes, from registration to discharge. To test their ideas, PHCS built a model patient room—not the usual rough mockup, but a fully functional patient room, right in the existing hospital—and provided patient care right there. “We made more than 200 changes,” says Rabner. Examples: putting a safe that could hold a laptop in the room, and installing a swivel night light next to the visitor’s couch to allow the patient to sleep.
The plan that eventually flowed from this process called for the main campus to be moved three miles out to a 171-acre site in suburban Plainsboro, where the new hospital would form the core of an elaborate mixed-use complex.
More important, the new PHCS University Medical Center at Plainsboro would step up its clinical capabilities through partnerships with nearby world-class institutions. The first of these is with Children’s Hospital of Philadelphia (CHOP). “My motto was, Don’t dabble,” says Rabner. “We were dabbling in pediatrics, and we determined that we would do better with a partner.” CHOP will build and staff a 100,000-sf clinic on the new campus; children needing more intense care will be transported to Children’s Hospital of Philadelphia.
PHCS had to go all out to sell the plan—which called for PHCS to divest the existing properties, including the old hospital—to the highly sophisticated Princeton community. “We had almost 75 meetings just on the strategic plan, and another 75 on the building design and zoning approval in Plainsboro Township,” says Rabner.
The logic of the plan turned the tide of opinion in PHCS’s favor. The old hospital has been sold to Princeton University, which will convert it into housing for faculty and staff. AvalonBay Communities bought the second site and will build apartments and keep the existing medical office building in operation.
The new 2.1-million-sf campus is being financed with cash from operations and the property sales, along with bonds and donations. The 630,000-sf University Medical Center at Plainsboro will offer nine centers of care, a 24-bed emergency department, eight labor/delivery rooms, 24 postpartum rooms, and 600-sf surgery suites.
In addition to the CHOP clinic, Formation-Shelbourne will build an 85-unit senior living complex, and Trammell Crow is putting in a five-story, 146,000-sf medical office building. Windsor Health has built a 200-bed skilled nursing facility and a subacute nursing facility, and will soon open a dialysis center. In the works: a 47,000-sf fitness/wellness center and a 13,000-sf childcare facility.
Rabner says he made “a big discovery” building the first new hospital of his career: “Before, I viewed a building as a container that holds people and equipment. I didn’t understand that the building has the capacity to help us reach our objectives.”
On May 22, he and his PHCS colleagues will find out how far they have progressed toward that goal. +
Related Stories
Mass Timber | Apr 22, 2024
British Columbia changing building code to allow mass timber structures of up to 18 stories
The Canadian Province of British Columbia is updating its building code to expand the use of mass timber in building construction. The code will allow for encapsulated mass-timber construction (EMTC) buildings as tall as 18 stories for residential and office buildings, an increase from the previous 12-story limit.
Standards | Apr 22, 2024
Design guide offers details on rain loads and ponding on roofs
The American Institute of Steel Construction and the Steel Joist Institute recently released a comprehensive roof design guide addressing rain loads and ponding. Design Guide 40, Rain Loads and Ponding provides guidance for designing roof systems to avoid or resist water accumulation and any resulting instability.
Building Materials | Apr 22, 2024
Tacoma, Wash., investigating policy to reuse and recycle building materials
Tacoma, Wash., recently initiated a study to find ways to increase building material reuse through deconstruction and salvage. The city council unanimously voted to direct the city manager to investigate deconstruction options and estimate costs.
Student Housing | Apr 19, 2024
$115 million Cal State Long Beach student housing project will add 424 beds
A new $115 million project recently broke ground at California State University, Long Beach (CSULB) that will add housing for 424 students at below-market rates. The 108,000 sf La Playa Residence Hall, funded by the State of California’s Higher Education Student Housing Grant Program, will consist of three five-story structures connected by bridges.
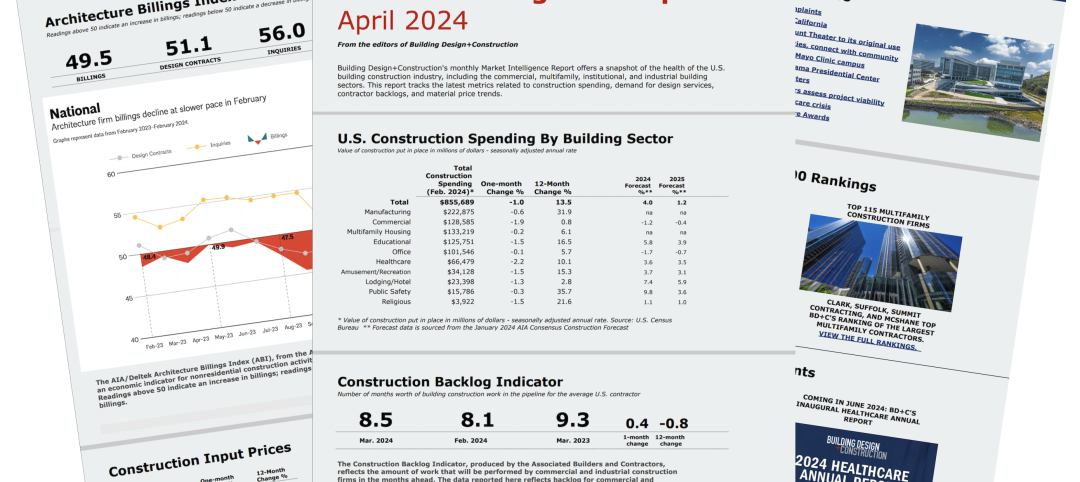
Construction Costs | Apr 18, 2024
New download: BD+C's April 2024 Market Intelligence Report
Building Design+Construction's monthly Market Intelligence Report offers a snapshot of the health of the U.S. building construction industry, including the commercial, multifamily, institutional, and industrial building sectors. This report tracks the latest metrics related to construction spending, demand for design services, contractor backlogs, and material price trends.
MFPRO+ New Projects | Apr 16, 2024
Marvel-designed Gowanus Green will offer 955 affordable rental units in Brooklyn
The community consists of approximately 955 units of 100% affordable housing, 28,000 sf of neighborhood service retail and community space, a site for a new public school, and a new 1.5-acre public park.
Construction Costs | Apr 16, 2024
How the new prevailing wage calculation will impact construction labor costs
Looking ahead to 2024 and beyond, two pivotal changes in federal construction labor dynamics are likely to exacerbate increasing construction labor costs, according to Gordian's Samuel Giffin.
Healthcare Facilities | Apr 16, 2024
Mexico’s ‘premier private academic health center’ under design
The design and construction contract for what is envisioned to be “the premier private academic health center in Mexico and Latin America” was recently awarded to The Beck Group. The TecSalud Health Sciences Campus will be located at Tec De Monterrey’s flagship healthcare facility, Zambrano Hellion Hospital, in Monterrey, Mexico.
Market Data | Apr 16, 2024
The average U.S. contractor has 8.2 months worth of construction work in the pipeline, as of March 2024
Associated Builders and Contractors reported today that its Construction Backlog Indicator increased to 8.2 months in March from 8.1 months in February, according to an ABC member survey conducted March 20 to April 3. The reading is down 0.5 months from March 2023.
Laboratories | Apr 15, 2024
HGA unveils plans to transform an abandoned rock quarry into a new research and innovation campus
In the coastal town of Manchester-by-the-Sea, Mass., an abandoned rock quarry will be transformed into a new research and innovation campus designed by HGA. The campus will reuse and upcycle the granite left onsite. The project for Cell Signaling Technology (CST), a life sciences technology company, will turn an environmentally depleted site into a net-zero laboratory campus, with building electrification and onsite renewables.