Healthcare facilities, especially our nation's hospitals, have steadily become larger over the past couple of decades. The growth has occurred despite stabilization, and in some markets, a decline in inpatient utilization. One measure of hospital size is Building Gross Square Feet (BGSF) per bed. BGSF is a measure of total facility envelope. Community hospitals built 30 years ago would typically range in the 1,300 - 1,600 BGSF per bed. However, today, a range of 2,200 - 2,800 BGSF per bed is not uncommon.
In today's healthcare environment, hospital leaders cannot afford to build these oversized facilities, but in some cases, they cannot afford not to. Healthcare executives delivering care in outdated 30+ year old facilities have to re-invest to meet new standards, keep up with competitors, and provide the services that are required in today's care environments. So what is going on here?
There are many factors influencing facility size with some of these changes being evolutionary and some being new and revolutionary (e.g. private rooms are evolutionary while hybrid ORs are new and revolutionary).
Inpatient Rooms Size and Occupancy
If you take a tour of an older hospital inpatient unit today, you will find rooms with multiple beds (two or three in some cases), no private toilet/shower room and little space for anyone but the patient. These rooms' sizes are in the 300 net square feet (NSF) range. Net square feet being the inside room dimension.
Today, private rooms are the norm and were actually recommended in the 2010 FGI Guidelines for Design and Construction of Healthcare Facilities. For a variety of reasons (patient privacy, infection control, patient preference), hospitals have moved away from multi-bed inpatient rooms. The size of these private inpatient rooms is typically between 260 - 320 NSF. The rooms include private toilet/showers; distinct zones for patient, caregiver, and family; and enough clear space for a variety of mobile technology that was not even dreamt of 50 years ago. Thus, the amount of NSF per patient in the room alone has just about doubled.
Facility Flexibility
Have you ever heard the terms Universal Room or Acuity Adaptable Room? These are rooms that either on a daily basis or with renovation can be utilized as a general medical/surgical room or as a Critical Care Unit (CCU) room. Given that the FGI Guidelines call for a minimum of 200 NSF of clear space for a CCU room and have requirements that the bed be one (1) foot from the wall with four (4) feet of clearance around the sides of the bed, new critical care rooms are rarely designed below 280 NSF today.
In an effort to standardize and provide a flexible bed chassis, hospitals are being designed and built with interchangeable room sizes for med/surg and CCU. Thus med/surg rooms are typically no less than 280 NSF. Any less, and acuity flexibility is compromised.
Privacy
In 1996 the Health Insurance Portability and Accountability Act (HIPAA) was enacted. This Act protects the privacy of individually identifiable health information. Since then, hospitals have re-tooled themselves to protect not only electronic information but what is spoken.
Americans culturally are modest people when compared to our European counterparts. This modesty extends into the hospital as well. As people sometimes say about Apple computers, "They just work," the same philosophy can be applied to private rooms, "They just make sense." When checking into a hotel, we are not paired in a two-bed room with some stranger that just happens to be staying at the hotel for the same nights. Why, when at our most vulnerable, during a time of extreme stress, are we placed in a room with someone else undergoing a similar physical and mental trauma? Privacy is more than just about the protection of information, it is about ensuring a clarity of focus for the care-givers, reducing nosocomial infections, ensuring quality rest free from roommate distractions, and protecting patient and family dignity during a stressful time. However, this privacy has come with some costs and benefits.
Privacy is not confined to the inpatient unit. Private rooms extend to the emergency department, peri-operative space (pre-op prep and phase II PACU), registration and admitting areas, and observation/Clinical Decision Units. This increases the space needed to care for patients. Square footage per patient increases to account for eliminating some economies of scale associated with sharing space as well as the need for door swings where there was once a pull curtain.
There is evidence that bed/room utilization and occupancy rates are higher in a private facility and lengths of stay are lowered thus increasing efficiency and throughput which helps off-set facility costs. Also, anecdotally, a market share and volume "bump" can be associated with private rooms as the market and patients respond positively to this new environment.
Hospital planners and designers are becoming more creative in sharing some of these private spaces. For instance, observation and emergency departments are typically busiest in the mid-afternoon, evening, and pre-dawn hours while peri-operative service spaces are typically busiest in the morning and early afternoon hours. Even though Prep and Phase II PACU rooms may be shared to account for utilization swings (prep in the morning, phase II PACU later), some are suggesting that a "universal care" room shared between ED, peri-op, and observation could minimize room down time and increase room utilization.
Sharing would decrease the total number of rooms required. This model is challenging to operationalize and has not been widely accepted - thus, time will tell.
Patients' Needs
The Americans with Disabilities Act (ADA) of 1990 changed the regulations related to the size of certain rooms in hospitals and outpatient settings (and other non-healthcare workplace areas as well). It is hard to believe that before 1990 there was little regulation regarding "accessible" spaces for those people most in need: healthcare patients. In hospitals, outpatient centers, and clinics nationwide, patients in wheelchairs, using walkers, visually and hearing impaired, or requiring some other source of assistance could not ambulate or use rooms in the building where they were receiving care. This juxtaposition did not go unnoticed and the facility codes have changed to allow "accessible" and ADA compliant space.
And it is not just for patients, but also for the public, families, and workforce in the buildings. 15 NSF closet size toilet rooms have been replaced with wheelchair accessible 50 NSF toilet rooms in patient care, public and staff areas. Exam rooms have increased in size from well under 100 NSF to a standard of 120 NSF to take into account accessibility, patient, and caregiver needs. Public spaces (lobbies, cafeterias, meeting rooms) provide more space per seat to allow for patient, public, and staff with disabilities to more freely travel and remove barriers to utilizations.
Obesity is also an American epidemic contributing to a host of co-morbid conditions (diabetes, hypertension, sleep apnea, etc.) that decrease the general health of the population and contribute to high utilization of health care services. Some 30%-35% of Americans are overweight, one of the highest rates of industrialized nations. Caring for the obese and bariatric patients requires oversized spaces and special equipment as evidenced in larger waiting room chairs, bariatric beds and wheelchairs, space for both mobile and fixed lift assist devices, and larger exam room doors.
Technology and Medical Equipment
Diagnostic and treatment spaces have increased over the years. A standard size for an operating room (OR) used to be approximately 450 - 480 NSF. Now, it is difficult to find a hospital OR being designed any less that 600 - 650 NSF. ORs have become larger given the more complex nature of cases being handled. These complex cases increased the number of care-givers in the room as well as the amount of equipment.
Computers, larger anesthesia carts, perfusion machines, integrated ceiling mounted monitors, robotic surgery consoles and mobile x-ray are just some of the equipment that are routinely brought into the OR. There needs to be room for all of this "stuff". Consider a hybrid or integrated imaging OR where interventional radiology equipment or MRI are fixed in the room, these ORs approach 800 - 1,000 NSF, not to mention the additional space needed for radiologic control and equipment.
The ubiquitous presence of large imaging equipment (MRI, PET, CT, etc.) and/or the increase in utilization and installation of linear accelerators are becoming standards-of-care and thus increasing the size of our healthcare facilities.
Physical Infrastructure Needs
The above are just a few of the reasons our facilities have grown over the last couple of decades. The physical envelopes that house all of the care and supportive space have also played a factor:
• Becoming a more connected platform, information technology has increased the need for server space, data centers, distributed MDF/data rooms, IT support and data analyst office space, which are now standard elements.
• The Evidence Based Design (EvBD) movement has increased the size of buildings and contributed to higher "grossing factors" (the amount of building space on top of departmental space) related to bringing in more natural light and separation of on-stage/off-stage space.
• The LEED/Sustainable Design movement as well as changes in environment of care codes promulgated by the Joint Commission and American Society for Healthcare Engineers (ASHE) has increased space related to infrastructure and increased floor to floor heights allowing for larger, but more energy efficient, mechanical equipment.
• The desire to create more standard, flexible, and "future-proof" inpatient and large ambulatory facilities has increased the size of the structural grid. Most facilities are being built on a 28' to 30' column bay. This increases overall size but provides a fungible footprint.
So, What Can You Do About It?
Healthcare executives, facilities managers, architectural and engineering, designers, planners, clinicians, and construction managers have responded by planning, designing, and building "right-sized" facilities utilizing some of the following tactics:
• Leveraging the System: As more and more independent hospitals continue to become part of an "Integrated Delivery System" it is not necessary to provide duplicative services across operating units. Non-direct care administrative services, information technology departments, full-service lab, pathology, and supply chain functions are being centralized to serve multiple operating units. This leaves space on hospital and ambulatory campuses for some core elements such as on-site "stat" and routine lab, a few Human Resource specialists, or emergency level stock to be included. This model is helping to increase efficiencies and reduce duplication.
• Improve Processes: Process improvement such as Lean and Six-Sigma is beneficial for eliminating waste. Streamlining and standardizing processes, clinical and supportive, helps designers to plan for only the rooms and space necessary for a particular function. Often, this can increase space by decentralizing elements, but may reduce overall space as functions are streamlined and the number of Key Planning Units (KPUs - e.g. beds, ORs, ED rooms) are planned at threshold and best-in-class throughput metrics. Consider leveraging technology in public spaces by offering items such as check-in kiosks (like at the airport) to reduce the need for large check-in and registration zones. It is more process and space efficient.
• Get Creative with Infrastructure: At a hospital in the mid-Atlantic, a modular central plant is being built for a much lower cost and in less space than a steel and concrete structure. This reduces space footprint cost and increases flexibility. Utilizing wireless technologies can reduce or eliminate the need for large data rooms. And, utilizing Building Information Management (BIM) technology when designing the building will most efficiently support mechanical, electrical, and plumbing infrastructure.
• Build for What is Needed: Reducing shell space and building enough capacity for "day one" operations and some modest growth is a solid planning strategy. Ensuring that capacity can be filled before expansion is prudent business in today's unsteady healthcare world. Working smart and planning for ready and easy expansion should be the approach. The last thing any healthcare organization wants today is big, empty, unutilized space.
All of the factors above that have increased the sizes of our healthcare facilities are ostensibly necessary as care delivery evolves. Privacy, creating a sustainable facility, and implementing new medical technologies are good for everyone. It is all about balance in today's cost-conscious environments. Whether it is for a large replacement hospital, off-site ambulatory care center, or primary care physician office, first provide what is needed then consider providing for wants. Creative design, leveraging health system resources, prudent planning, integrated program/project management, and providing for efficient operations will help ensure functional, flexible, and efficient right-sized facilities.
Related Stories
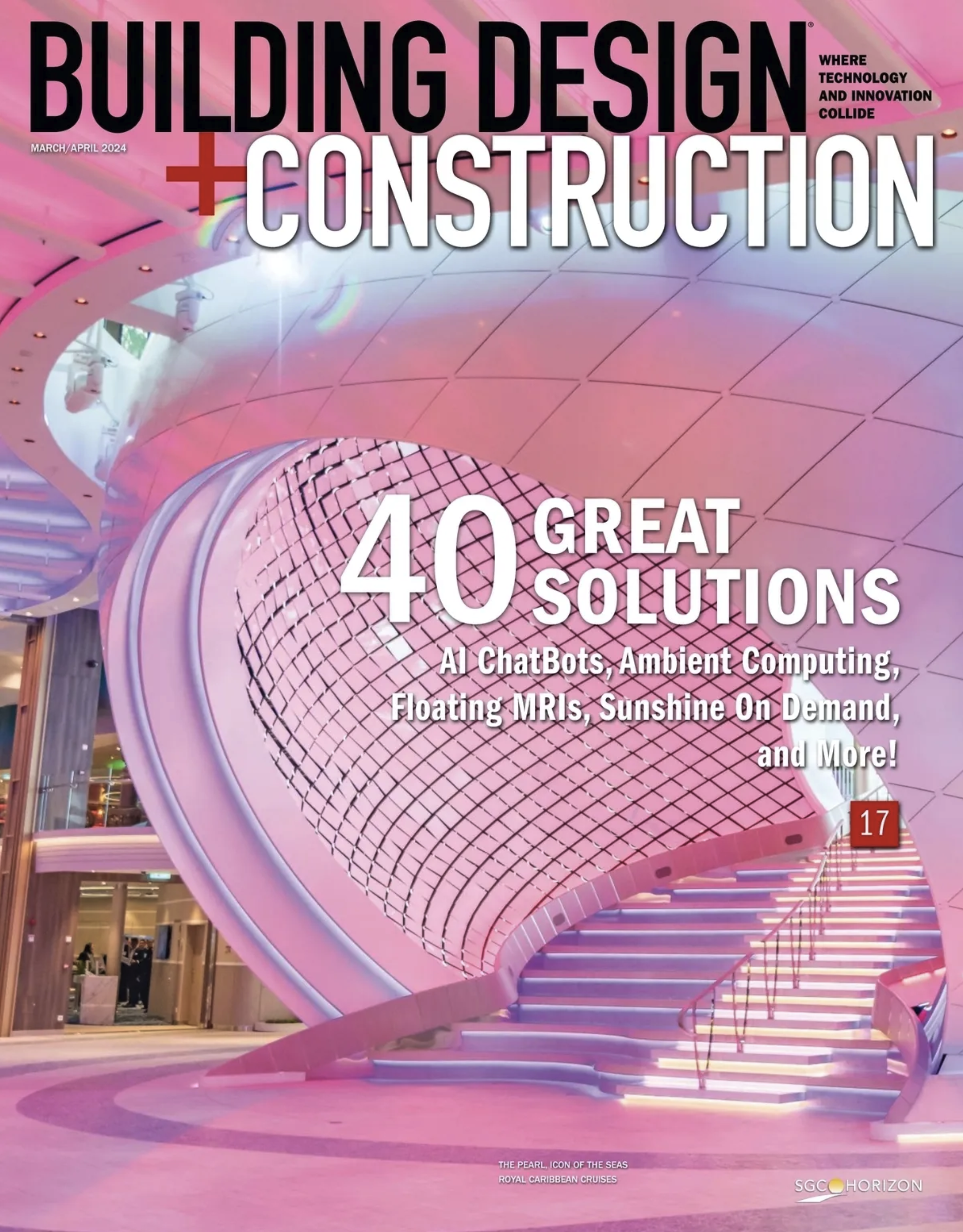
Shopping Centers | Mar 7, 2024
How shopping centers can foster strong community connections
In today's retail landscape, shopping centers are evolving beyond mere shopping destinations to become vibrant hubs of community life. Here are three strategies from Nadel Architecture + Planning for creating strong local connections.
Market Data | Mar 6, 2024
Nonresidential construction spending slips 0.4% in January
National nonresidential construction spending decreased 0.4% in January, according to an Associated Builders and Contractors analysis of data published today by the U.S. Census Bureau. On a seasonally adjusted annualized basis, nonresidential spending totaled $1.190 trillion.
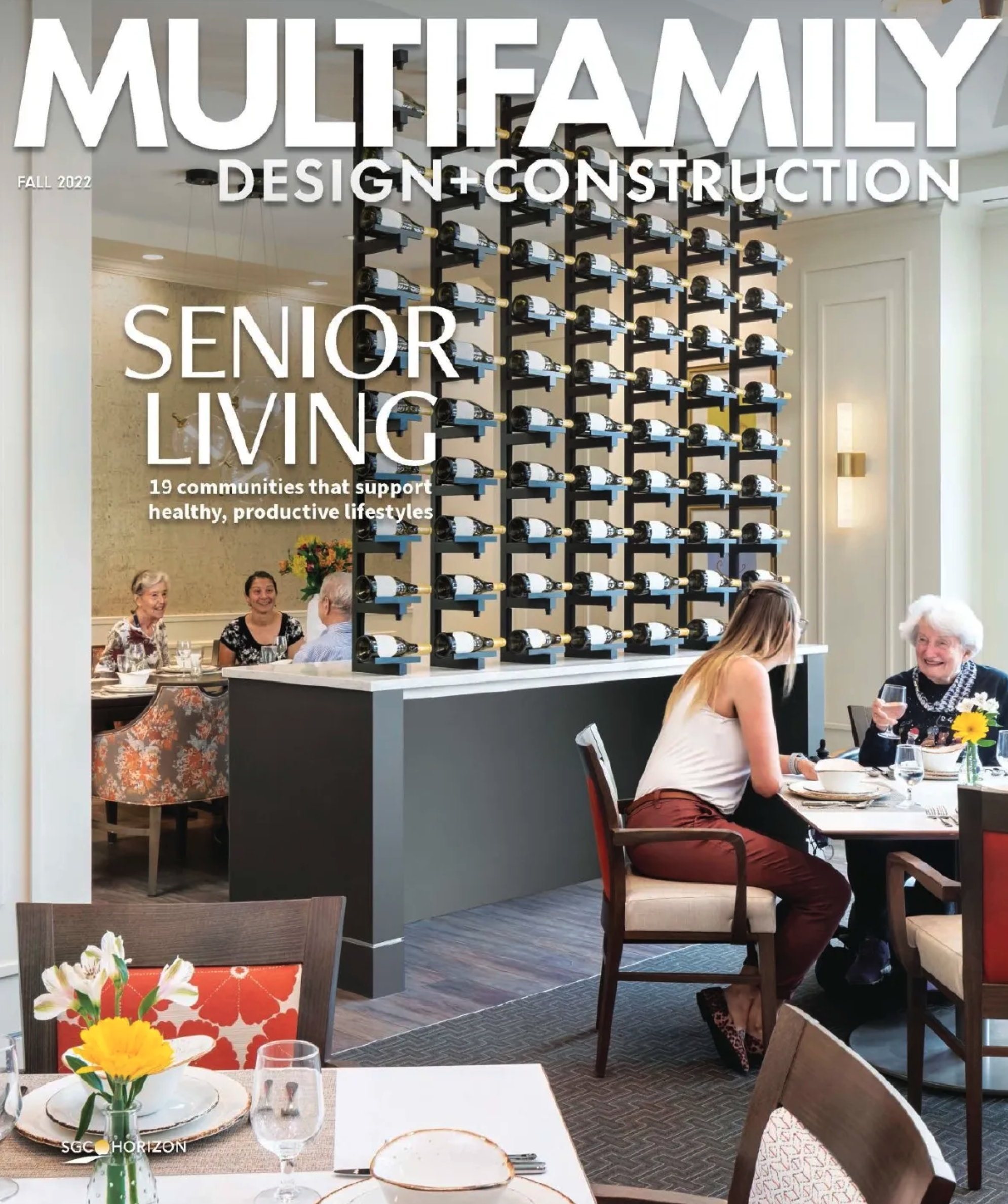
MFPRO+ Research | Mar 6, 2024
Top 10 trends in senior living facilities for 2024
The 65-and-over population is growing faster than any other age group. Architects, engineers, and contractors are coming up with creative senior housing solutions to better serve this burgeoning cohort.
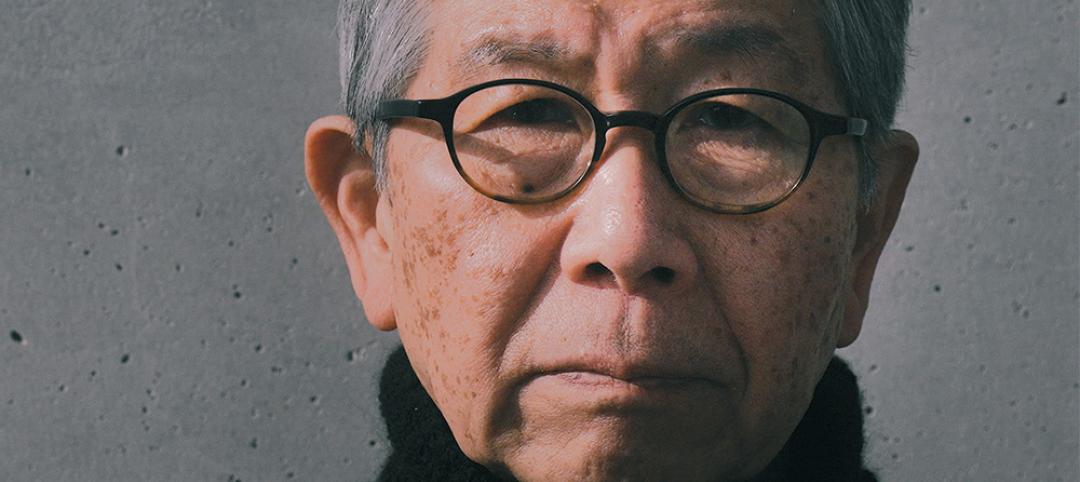
Architects | Mar 5, 2024
Riken Yamamoto wins 2024 Pritzker Architecture Prize
The Pritzker Architecture Prize announces Riken Yamamoto, of Yokohama, Japan, as the 2024 Laureate of the Pritzker Architecture Prize, the award that is regarded internationally as architecture’s highest honor.
Office Buildings | Mar 5, 2024
Former McDonald’s headquarters transformed into modern office building for Ace Hardware
In Oak Brook, Ill., about 15 miles west of downtown Chicago, McDonald’s former corporate headquarters has been transformed into a modern office building for its new tenant, Ace Hardware. Now for the first time, Ace Hardware can bring 1,700 employees from three facilities under one roof.
Green | Mar 5, 2024
New York City’s Green Economy Action Plan aims for building decarbonization
New York City’s recently revealed Green Economy Action Plan includes the goals of the decarbonization of buildings and developing a renewable energy system. The ambitious plan includes enabling low-carbon alternatives in the transportation sector and boosting green industries, aiming to create more than 12,000 green economy apprenticeships by 2040.
Lighting | Mar 4, 2024
Illuminating your path to energy efficiency
Design Collaborative's Kelsey Rowe, PE, CLD, shares some tools, resources, and next steps to guide you through the process of lighting design.
MFPRO+ News | Mar 1, 2024
Housing affordability, speed of construction are top of mind for multifamily architecture and construction firms
The 2023 Multifamily Giants get creative to solve the affordability crisis, while helping their developer clients build faster and more economically.
Multifamily Housing | Feb 29, 2024
Manny Gonzalez, FAIA, inducted into Best in American Living Awards Hall of Fame
Manny Gonzalez, FAIA, has been inducted into the BALA Hall of Fame.
K-12 Schools | Feb 29, 2024
Average age of U.S. school buildings is just under 50 years
The average age of a main instructional school building in the United States is 49 years, according to a survey by the National Center for Education Statistics (NCES). About 38% of schools were built before 1970. Roughly half of the schools surveyed have undergone a major building renovation or addition.