America’s healthcare sector found itself in an ambivalent state in late 2020, as the coronavirus raged relentlessly across the country and as the distribution of two newly approved vaccines started rolling out to inoculate vulnerable population groups.
Coronavirus-related expenses had already leveled a financial blow to healthcare systems. The American Hospital Association expected hospital losses for 2020 to exceed $323 billion. The pandemic accentuated the need for flexible healthcare and research facilities and services that can address present and future crises. Healthcare, in fact, was one of the few nonresidential building types that showed year-to-year increases in construction spending over the first 10 months of 2020, according to Census Bureau estimates.
The pandemic, say AEC sources, creates opportunities for design and construction, as healthcare systems continue to move their services closer to where patients live, and as operators look for ways to “futureproof” their facilities to meet whatever comes next.
Contagion-control and safety protocols put in place at the onset of the pandemic are becoming standard for new projects and renovations. Alternate forms of patient care—particularly telehealth—are being embraced. And to get buildings and services up and running quicker, developers, owners and their AEC partners are more open to considering different project delivery methods that lean toward early team collaboration.
OUTPATIENT FACILITIES DRIVE CONSTRUCTION
First and foremost, new healthcare projects are being initiated in response to local population growth and needs.
On December 17, the construction firm Robins & Morton and South Texas Health System broke ground on a five-story 150,000-sf patient tower in Edinburg, Texas, in that state’s bustling Rio Grande Valley. When completed in mid 2022, this Gresham Smith-designed tower will contain 15 exam rooms, two trauma rooms, four triage rooms, 16 suites, 28 inpatient rehab suites, 15 med-surg suites and space for future expansion. Another 20,000 sf are being renovated within the existing building to update its catherization lab, pharmacy, and other lab spaces.
“In general, healthcare is very strong nationally, and we’re still seeing [demand] for mega projects,” says Barbara Wagner, Executive Vice President with Clark Construction. On the day that BD+C interviewed Wagner (December 10), Clark had received an RFP for $300 million of construction on a $1 billion hospital project. In the previous 12 months, her firm’s healthcare work included billion-dollar projects for Stanford University and Fort Bliss in Texas.

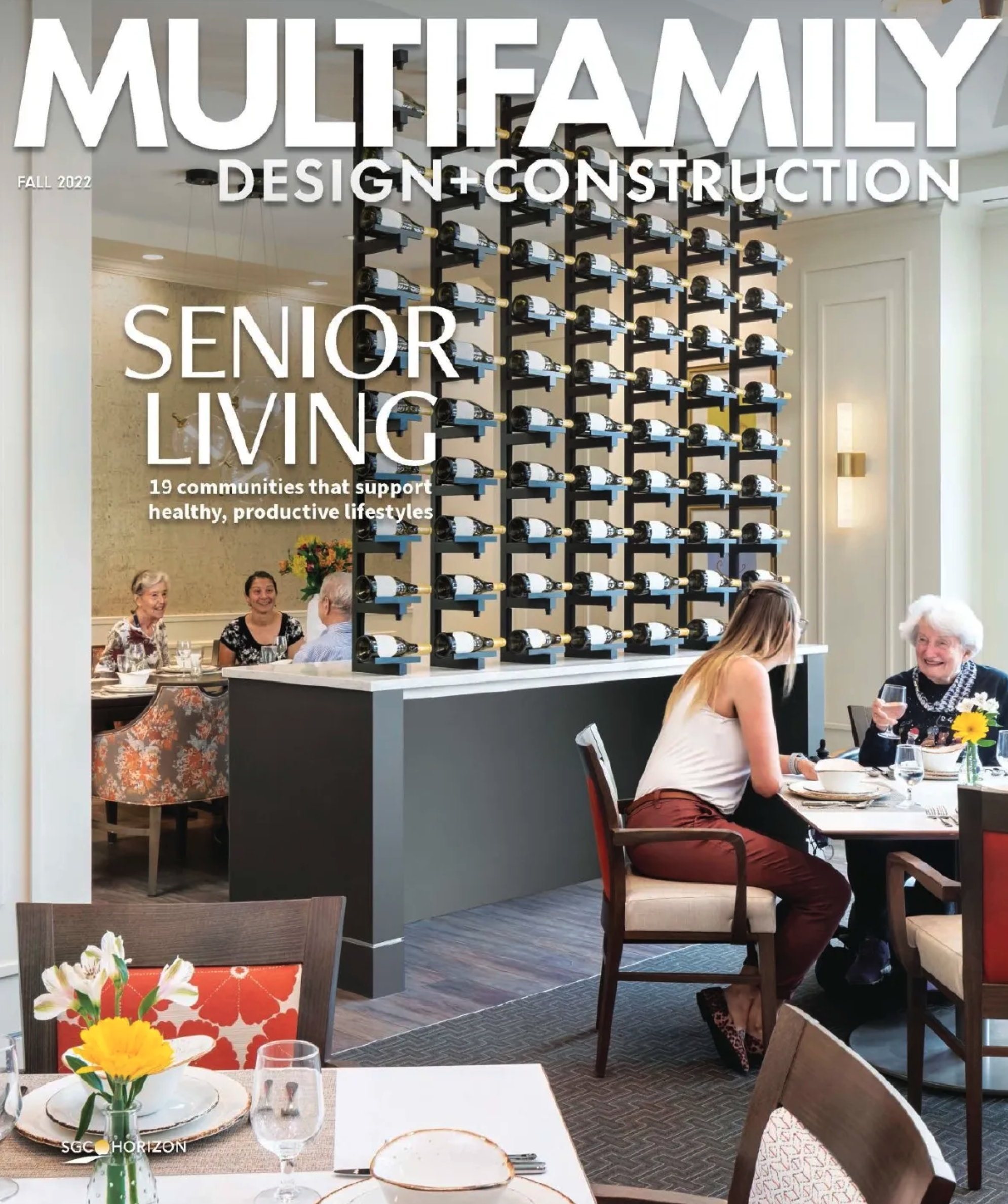
The Los Angeles County + University of Southern California Restorative Care Village project—for which CannonDesign provided design, engineering, and construction services—is home to a comprehensive strategy for managing the whole-person and full continuum of challenges facing vulnerable populations with serious medical, mental health, and addiction problems. Its Recuperative Care Center, with 96 beds, handles individuals discharged from inpatient hospitals. Its four-building, 64-bed Residential Treatment Program provides a short-term alternative to hospitalization. Courtesy CannonDesign
Wagner adds that there have been more federally funded healthcare projects now that the Veterans Administration and the Army Corps of Engineers are working together.
Other AEC firms say that healthcare demand varies by market; in Chicago, it’s for cancer centers; in Florida, where there are 4.4 million residents age 65 or older, inpatient hospital beds are always needed.
That being said, AEC sources say demand for outpatient facilities is driving the lion’s share of their healthcare work, “especially those [facilities] with a range of services,” says Tammy Ng, LEED AP BD+C, Project Manager and Associate with MBH Architects in San Francisco. A report that Deloitte posted in February 2020 estimated that outpatient services accounted for 48% of healthcare systems’ revenue in 2018, a figure that almost assuredly increased over the following two years.
The outpatient phenomenon is part of a larger trend where healthcare systems are pushing their services closer to neighborhoods those systems serve. That trend explains the growth in microhospitals with emergency departments and 10 to 12 beds, says Brad Earl, AIA, NCARB, SSGB–Healthcare, Managing Principal at Nelson Worldwide’s healthcare architecture studio in Philadelphia.
In the New York metro area, Al Thompson, Managing Executive and Studio Director for TPG Architecture, says his firm has seen more interest in what he calls concierge-type services for high-net-worth patients. TPG recently received three RFPs for such fit-outs inside medical office buildings in Manhattan, which would include equipment for MRIs, CT scans, X-rays, and other specialty services.
HEALTHCARE'S FUTURE IS FLEXIBLE SPACE
Perkins and Will recently conducted roundtable discussions with clients, during which one Human Resources manager in Nebraska said that her system was considering casting its hiring net nationally because people don’t have to live in Nebraska to do certain healthcare jobs anymore. “The seeds of these ideas could have long-lasting roots,” predicts Scott Davidson, AIA, NCARB, P&W’s Midwest health and Wellness Practice Leader.
The coronavirus pandemic has led many healthcare owner-operators to rethink their current and future space needs. “Clients are pulling back and tearing apart” their buildings, trying to figure out what is and isn’t essential, observes Aran McCarthy, AIA, NCARB, Principal–Healthcare for Francis Cauffman Architects (FCA).
These re-evaluations have opened doors for more flexible design options that include adaptive reuse. MBH, for example, has done design work for longtime client On Lok—a nonprofit that provides medical, nutritional, and social service plans that allow seniors to stay in their homes longer—to convert various building types for its centers.

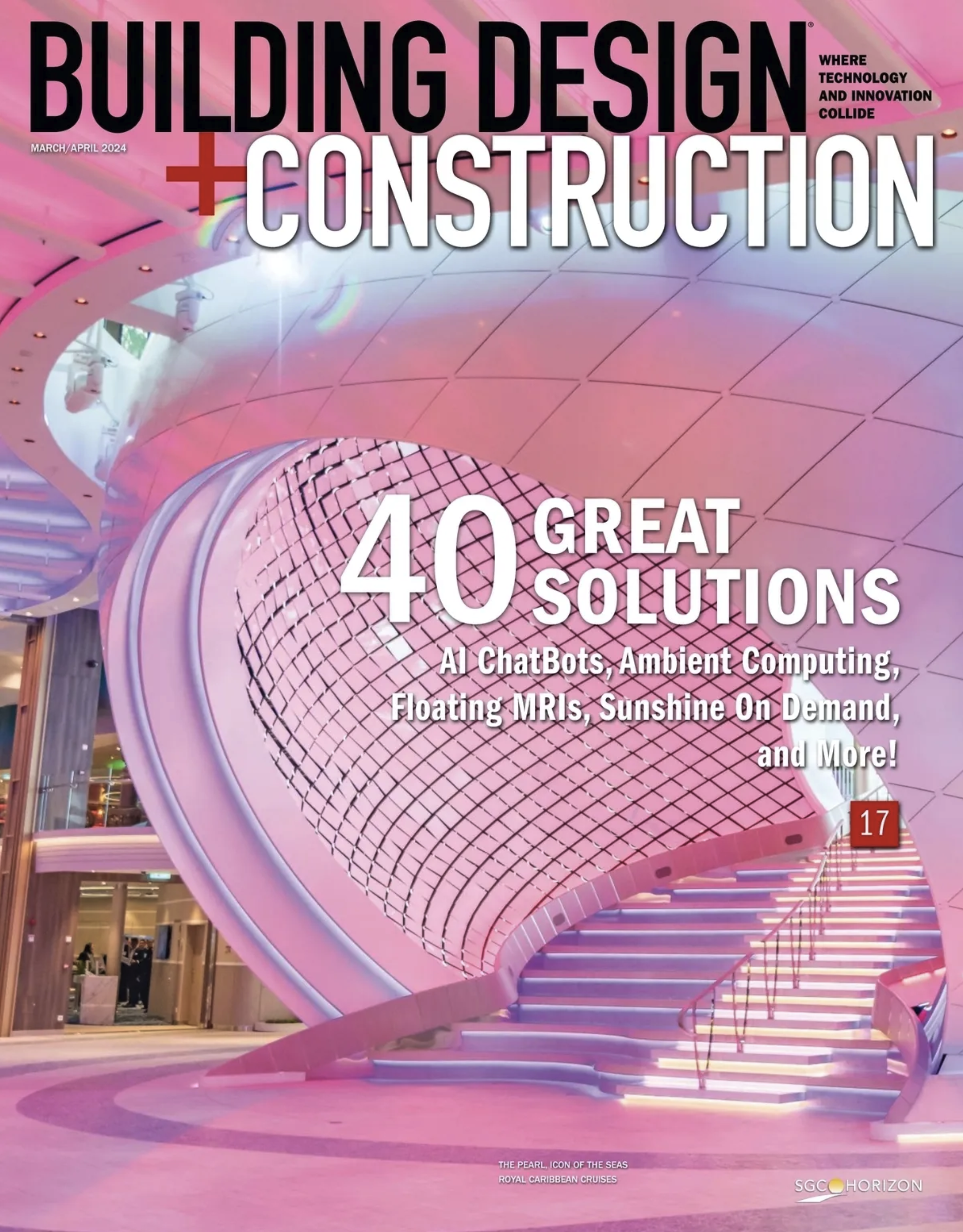
Demand for facilities that offer behavioral health treatment is expanding. Strawberry Hill Behavioral Health Hospital, part of the University of Kansas Health System, opened in Kansas City, Kan., in October 2019. It includes a four-story central atrium with planter beds and vertical green walls. The outdoors is never too far from patients in any of the hospital’s spaces. Photo: Laura Peters
One of CannonDesign’s recent projects is the 105,000-sf Strawberry Hill Behavioral Hospital in Kansas City, Kan., part of the University of Kansas Health System. This project, which was completed in the fall of 2019, converted a vacant government office building to an inpatient hospital whose units are flexible: they can be made into single 24-bed units, or rearranged to include two or three times that number of beds by controlling a series of cross-corridor doors.
“The pandemic has emphasized how important it is to be ready for anything,” says Abbie Clary, AIA, FACHA, LEED AP, who directs CannonDesign’s Health Practice.
With the aid of technology, this sector is moving away from the physical exam always being the center of the patient’s healthcare experience. “We need to find ways to maintain the human touch aspect of healthcare,” says Derek Veilleux, AIA, EDAC, NCARB, Senior Principal and Director of Health & Wellness Practice for SMRT Architects & Engineers. He believes design can play a role in fostering stronger connections between patients and providers.
Veilleux predicts that patient screening areas are here to stay at the entrances of medical office buildings, and that waiting rooms in MOBs will eventually give way to having patients wait in individual exam rooms.
Regardless of their determinations about space, owner-operators are more concerned than ever about making their facilities as germ-free as possible. “During the pandemic, there was an awareness that most healthcare facilities lacked the infrastructure design to be quickly and efficiently converted to serve the needs of infection control for this type of disease,” asserts Fawn Staerkel, Johnson Controls’ Healthcare Director of Strategic Accounts. Consequently, the pandemic triggered a “dramatic need” for building controls, improved air quality, greater HVAC capability, and overall facility resilience.
Several AEC sources interviewed for this article say their clients are demanding designs and engineering that allow hospital units to adjust quickly to different health situation. One of Robins & Morton’s projects coming out of the ground near Tampa, Fla., will include a 42-bed med-surg unit that can be converted to isolation rooms “with the flip of a switch,” says Bruce Adams, a Vice President with the firm.
“Futureproofing” is now part of most healthcare systems’ planning lexicons. “Every aspect of each facility, from arrival to discharge, is being reviewed and reconsidered when designing new or renovated space,” says Brian Hamilton, Consigli Construction’s Director of Healthcare and Life Sciences.
THE NEED FOR SPEED IN HEALTHCARE DESIGN AND CONSTRUCTION
During the pandemic, AEC firms and the healthcare clients stepped to the plate when it came to constructing emergency facilities quickly. That “speed to market” mentality now permeates all healthcare projects, even though there’s no real consensus about which delivery method is most efficient.
Adams of Robins & Morton believes that CM at risk is still the fastest way to get projects started. He points as an example to the aforementioned project near Tampa, the $246 million 86-bed BayCare Hospital in Wesley Chapel with medical office buildings attached, which is scheduled for completion in early 2023. Even though the design documents weren’t ready until November 2020, Robins & Morton had been working on the project for four months. “It’s a matter of winning the client’s confidence” that the project will stay within budget and on time, Adams says.
He adds, though, that between 15% and 20% of his firm’s work is executed under alternate delivery contracts. CannonDesign’s Clary notes that there’s “great interest” among clients in newer delivery models that can accelerate projects. These include Integrated Project Delivery (IPD), Progressive Design Build (PDB), and Modular Design and Construction. “The scope of work documents can no longer be contained between disparate contracting chains,” says Staerkel of Johnson Controls.
Rich Steimel, Principal in charge of Healthcare for Lendlease, proclaims himself a “huge fan” of IPD, which has been the model his firm has used for the past three years for work it’s performed for the Mt. Sinai hospital system in New York.
SMRT considers itself a leader in alternate delivery methods, and currently is engaged in a design-build partnership in Georgia with a construction management firm that it previously completed an IPD project with. “We are leveraging our strong relationships to push the envelope and explore new opportunities to the benefit of our clients,” says Veilleux.
SEE ALSO: As mental healthcare is destigmatized, demand for treatment centers is rising

The demand for healthcare facilities that offer mental and behavioral health services is increasing, and presents new design and construction opportunities to AEC firms. Read the story
McCarthy cautions, however, that IDP “is not for every client.” FCA has found that benefits are most evident on projects that are $10 million or higher.
Progressive Design Build, which the Design-Build Institute of America formulated about a decade ago, has attracted advocates in recent years. This contract type involves the design-build team at the earliest stages of a project’s development. And unlike some other alternate delivery contracts, the design-builder under PDB can be chosen almost entirely on qualifications.
One of Clark Construction’s current PDB projects (in a JV with Abbott Construction) is a healthcare facility for the University of Washington in Seattle that will include mental and behavioral health services in rooms that could be converted to med-surg units as needed. Wagner says that 30 architectural firms were interviewed for this project, and the state chose SRG Partnership from four finalists primarily because the person that SRG would assign to the project team had solid behavioral health experience. (The team is scheduled to submit its Guaranteed Maximum Price for this project in July, and it should be completed by 2023.)
PREFAB AND MODULAR SOLUTIONS HELP FIRMS KEEP PACE WITH DEMAND
The pandemic has certainly raised healthcare clients’ expectations about what’s doable. In early 2020, Taikang Tongji Hospital in Wuhan, China, urgently hired Johnson Controls to install the necessary infrastructure to support 300 beds to treat COVID-19 patients. Within days of completing that work, the hospital said it needed to support another 600 beds. Johnson Controls mobilized its team within 12 hours of that request, and 20 hours later started construction. Over the next 72 hours, a shelter hospital had been rebuilt to include safety and communications systems. And within the next three days, Johnson Controls had equipped 860 beds with medical intercom and nurse call systems.
Last summer, SMRT, working with Landry/French Construction and their client Abbott Laboratories, completed in just in two months the adaptive reuse of an industrial park building in Scarborough, Maine, to a 126,072-sf diagnostic lab that produces COVID-19 tests. That conversion time was 10 months faster than a pre-pandemic facility reconstruction might have taken, says Veilleux.
AEC firms with healthcare practices appear to be managing manpower availability for design and construction somewhat better than other sectors. Consigli Construction has been hiring subcontractors under Design-Assist contracts that allow for detailed coordination and material procurement much earlier in the process, says Hamilton.
But the pandemic has made it more difficult to keep up with owner-operators’ demands to get buildings online quicker. To that end, prefabrication and modularity have become more prominent tools. Earl of Nelson Worldwide points to EIR Healthcare’s MedModular—launched in September 2018 as the first application of prefabrication and modular technology for hospital rooms that can be delivered 90% complete—as an example of solutions that are gaining traction.
Perkins and Will is the architect on the 38,206-sf tower addition to MHealth Fairview’s Southdale Hospital in Edina, Minn., that is adding 48 beds. Davidson, P+W’s Practice Leader, says the structural steel for this project was prefabricated. And on one recent healthcare project, Lendlease partnered with the prefab wall supplier DIRTT, whose product, says Steimel, was “faster [to install] and more complete” than conventional building methods.
To address its clients’ requests for speedier delivery, CannonDesign has added new service lines: Blue Cottage (health consulting), ModularDesign+ (which Clary describes as a “breakthrough” design and construction company), and CD Builders (to advance new project delivery methods). Modular design accelerated the timeline for one of CannonDesign’s projects, the Los Angeles County and University of Southern California Restorative Care Village, a healthcare campus scheduled to open in 2021. Largely modular, with prefab materials and spaces, this campus will include a recuperative care center with 96 beds, and a four-building 64-bed residential treatment program that provides alternatives to hospitalization.
A TIME OF CHANGE FOR HEALTHCARE DESIGN
Davidson of Perkins and Will fully expects the healthcare sector “to feel normal again” by the third quarter of 2021. But given how the pandemic destabilized the U.S. economy, uncertainty remains. Wagner says that Clark Construction has been working with Cedars-Sinai on a $300–$400 million tower that the hospital is wary about starting because of the economy.
Some things about the future, though, seem surer to AEC firms:
Telehealth will continue to expand. “I have not seen a healthcare system that hasn’t embraced this,” says Wagner. Clary of CannonDesign suggests that the current evolution of telemedicine could attract and establish new patient-provider relationships beyond a system’s immediate market reach, perhaps into rural areas where services are often in short supply.
The demand for behavioral healthcare services will increase. Consigli’s Hamilton says his firm is already seeing an “uptick” in new behavioral health facilities being built and planned for. But Davidson cautions that expansion will depend on the healthcare system’s mission. “These services generally aren’t money makers, but could have longer-term benefits by keeping patients out of EDs,” he says.
SMRT’s Veilleux notes that U.S. hospitals spend $8.8 billion annually on energy. Their energy consumption is typically three times that of other commercial buildings. At a time when the pandemic has rendered many healthcare systems financially fragile, he anticipates that more attention will be paid to controlling their energy use.
Veilleux also expects systems to place more emphasis on nonclinical and -medical components and spaces that support community partnerships, such as adult day health facilities that allow people to stay in their homes longer.
As the delivery of healthcare services relies more on technology, systems will need to help their patients—especially less-tech-savvy seniors—reach a certain level of adeptness. FCA’s McCarthy singles out Atlantic Health Morristown (N.J) Medical Center’s “HealtheConnect” service that offers support of a full-time specialist who assists patients to use health-specific mobile applications.
On a broader operational scale, Staerkel of Johnson Controls sees “command centers” gaining momentum as healthcare facilities try to leverage available data into actionable and meaningful outcomes. “These command centers are powering telehealth solutions, enabling doctors around the world to consult and maintain visibility to a remote patient’s condition, and act as the central call center for the facility or system,” says Staerkel.
Related Stories
Sponsored | | Jul 12, 2023
Keyless Security for Medical Offices
Keeping patient data secure is a serious concern for medical professionals. Traditional lock-and-key systems do very little to help manage this problem, and create additional issues of their own. “Fortunately, wireless access control — a keyless alternative — eliminates the need for traditional physical keys while providing a higher level of security and centralized control,” says Cliff Brady, Salto Director of Industry Sectors Engagement, North America. Let’s explore how that works.
Healthcare Facilities | Jul 10, 2023
The latest pediatric design solutions for our tiniest patients
Pediatric design leaders Julia Jude and Kristie Alexander share several of CannonDesign's latest pediatric projects.
Healthcare Facilities | Jun 27, 2023
Convenience ranks highly when patients seek healthcare
Healthcare consumers are just as likely to factor in convenience as they do cost when deciding where to seek care and from whom, according to a new survey of 4,037 American adults about their attitudes and preferences as patients. The survey, conducted from April 19-28 by JLL, in many ways confirms the obvious: that older generations seek preventive care more often than younger generations; that insurance coverage is a primary driver for choosing a provider or hospital; and that the quality of service affects the patient experience.
Healthcare Facilities | Jun 27, 2023
A woman-led CM team manages the expansion and renovation of a woman-focused hospital in Nashville
This design-build project includes adding six floors for future growth.
Standards | Jun 26, 2023
New Wi-Fi standard boosts indoor navigation, tracking accuracy in buildings
The recently released Wi-Fi standard, IEEE 802.11az enables more refined and accurate indoor location capabilities. As technology manufacturers incorporate the new standard in various devices, it will enable buildings, including malls, arenas, and stadiums, to provide new wayfinding and tracking features.
Healthcare Facilities | Jun 14, 2023
Design considerations for behavioral health patients
The surrounding environment plays a huge role in the mental state of the occupants of a space, especially behavioral health patients whose perception of safety can be heightened. When patients do not feel comfortable in a space, the relationships between patients and therapists are negatively affected.
Engineers | Jun 14, 2023
The high cost of low maintenance
Walter P Moore’s Javier Balma, PhD, PE, SE, and Webb Wright, PE, identify the primary causes of engineering failures, define proactive versus reactive maintenance, recognize the reasons for deferred maintenance, and identify the financial and safety risks related to deferred maintenance.
Healthcare Facilities | Jun 5, 2023
Modernizing mental health care in emergency departments: Improving patient outcomes
In today’s mental health crisis, there is a widespread shortage of beds to handle certain populations. Patients may languish in the ED for hours or days before they can be linked to an appropriate inpatient program.
Healthcare Facilities | Jun 1, 2023
High-rise cancer center delivers new model for oncology care
Atlanta’s 17-story Winship Cancer Institute at Emory Midtown features two-story communities that organize cancer care into one-stop destinations. Designed by Skidmore, Owings & Merrill (SOM) and May Architecture, the facility includes comprehensive oncology facilities—including inpatient beds, surgical capacity, infusion treatment, outpatient clinics, diagnostic imaging, linear accelerators, and areas for wellness, rehabilitation, and clinical research.
Healthcare Facilities | May 19, 2023
A new behavioral health facility in California targets net zero energy
Shortly before Mental Health Awareness Month in May, development and construction firm Skanska announced the topping out of California’s first behavioral health facility—and the largest in the nation—to target net zero energy. Located in Redwood City, San Mateo County, Calif., the 77,610-sf Cordilleras Health System Replacement Project is slated for completion in late 2024.