Our healthcare system has been pushed beyond capacity by the ever-growing number of COVID-19 patients. The need for hospital beds, ventilators, PPE, and isolation rooms has vastly outstripped the available supply, and the country is looking for spaces to repurpose into healthcare service. Our team of healthcare experts, along with design experts across diverse building types and engineering disciplines, can help convert existing buildings such as hotels, convention centers, and arenas into temporary healthcare facilities. We understand not only the infection-control requirements needed to convert these spaces, but also the existing infrastructure and functional layout of them. Having knowledge of both is crucial for success when making modifications to repurpose these environments to care for the sick among us.
Many of these building types are not an obvious fit for a healthcare space. As we mentioned in our previous article on negative isolation rooms, there are specific airflow requirements in place to minimize the chances of cross-contamination to caregivers and other patients when designing infrastructure serving an infectious patient. Supporting patients suffering from COVID-19 requires even further design consideration since many patients may need ventilators. Ventilators require oxygen piped from a medical gas system and must have electrical systems provided by emergency power circuits to ensure they will continue to operate in the event of a power failure. The typical requirements for negative isolation rooms, medical gas, and emergency power are not always easy to implement in alternative building sites, but it is possible.
Below we will discuss the following building types being converted into temporary hospital spaces and address some of the challenges and opportunities that exist in each. In all situations, discussions with the owner-operator and design/construction team will be critical to understand the patients who will be in these types of facilities and their needed level of care. The building types are:
- Hospital Conversion Spaces
- Temporary Modular Space Design/Conversions
- Hotel/Student Residence Conversions
- Convention Center/Arena/Auditorium Conversions
HOSPITAL CONVERSION SPACE
Converting hospital spaces to serve infectious patients may seem more straightforward than other building types discussed below; however, there are still many considerations to think through.
- Patient Isolation Room Conversions: Most patient rooms return air back to the main HVAC system – typically an air handling unit (AHU) – in lieu of exhausting directly to the exterior as is required in isolation rooms. In single-story buildings, intercepting a return air main and connecting it to an exhaust fan can be relatively simple if the return is only serving patient rooms. Even in this arrangement though, the patient’s restroom exhaust would need to be modified to remove any exhaust from non-isolation spaces. If patient restroom exhaust modifications are not possible, a decision should be made regarding the risk of not exhausting the toilet room against the possibility of cross-contamination should the fan shut down.
- Negative Pressure Rooms: Maintaining a room at negative pressure is one of the most critical factors to minimizing cross-contamination. If the retrofit is in an exterior room, the airflow will most likely be close to 12 ACH with no modifications. In these cases, the supply air would be reduced to provide the room negative pressure if the return cannot be increased appropriately.
- Air Flow Considerations: If a room is cooled utilizing a recirculation room unit, such as fan coils or induction units, the room exhaust should be isolated from all other spaces and increased to the largest amount possible to create the negative pressure. Alternative technologies to sanitize the space should be considered in spaces with recirculating room units. Typically, an existing AHU is not sized to accommodate the quantity of outdoor air necessitated by exhausting all rooms served by the AHU. Additionally, the existing HVAC system cannot always be replaced or upgraded (to add increased capacity) in a cost-effective or quick manner. If the system is not able to adequately cool the air humidity, issues may present themselves in summer months, creating additional challenges in the healing process. Providing a dedicated outdoor air unit to precool a portion of the outdoor air can help alleviate these concerns.
- Electrical & Med Gas Infrastructure: If an existing patient room is being converted, the electrical and medical gas infrastructure should be able to be reused in most cases. That said, high ventilator usage in a facility could, potentially, tax the oxygen system sizing due to diversity factors typically assumed in the design of healthcare spaces.
Even though infectious disease is on the top of everyone’s mind right now, it is important to remember that other medical conditions require continued treatment throughout this time. Taking precautions to separate these patients from patients with infectious diseases is critical to ongoing health. Separating wings or units of the hospital for standard patient use by utilizing air locks to prevent transition of viruses is crucial. We must also limit access to these areas to specific staff and visitors (when necessary). Increasing filtration or utilizing alternate technologies in air handling equipment can help prevent cross-contamination to other parts of the building.
TEMPORARY MODULAR SPACE DESIGN/CONVERSION
Utilizng temporary or modular structures to increase patent care areas has several advantages because it separates the infectious patients from other patients. These spaces can also be customized for a specific region or patient population, and as modular structures they can be quickly disassembled and reassembled to change location as needed. These spaces can range from a trailer with individual pods for patients to a larger open room with beds and separate work areas for caregivers.

-
Air Flow Considerations: If infectious patients are in these spaces, they would not typically have rooms sized as large as a standard patient room or the individual occupant HVAC, lighting, or entertainment controls. These spaces should be provided with a 100 percent outside air (OSA) unit to allow all interior air to be exhausted to the roof of the structure with HEPA filtration. Air flow will be critical to keep cross-contamination at a minimum. In an open room with beds and a central walkway, the clean supply air should be delivered over the walkway and near where caregivers enter the patient treatment space. The exhaust should duct to the exterior and terminate low on the wall near each bed. This arrangement will encourage airflow patterns that keep contamination near the source and draws the conditioned air to the patient to maintain comfort. The outdoor air unit should be sized to dehumidify the outdoor air so than the space conditions encourage the cleanest environment.

- Electrical & Med Gas Infrastructure: Medical gases also will need to be extended to the facility to provide patient care. If this temporary facility is near an existing hospital, the bulk oxygen tank may provide a connection point for the temporary facilities. The existing vaporizers and size will need to be evaluated and frequency of fill increased to account for the increased number or patients. Utilizing medical gas cylinders for patients may be an option if a bulk oxygen plant is not available. Other utilities will also need to be provided to the temporary facility. Power, with generator back-up, supporting the HVAC and life safety equipment is necessary, as well as technology (often network fiber) to provide communication with family members and healthcare providers.
HOTEL/STUDENT RESIDENCE CONVERSION
Hotels provide perhaps the most feasible locations for temporary healthcare facilities because they offer individual rooms with private restrooms, which can help prevent cross-contamination. Hotels also have an existing technology infrastructure to allow communication with family and healthcare providers, and they have food service functions to provide a staging area for patients’ dietary needs. College residences have similar infrastructure already in place as well. However, there are still several hurdles to overcome when converting these spaces into a safe environment for the healthcare provider.
- Air Flow/Exhaust System Considerations: These facilities do not have the capability of exhaust air at the level required for infectious disease rooms and typically utilize recirculating room units with minimal outdoor air. The exhaust systems at these facilities likely needs to be upgraded to provide the required airflow to maintain a negative pressure in the space. If this cannot be accommodated due to the existing infrastructure, an exhaust fan with HEPA filter could be extended out of the sidewall or window and balanced to maintain a negative pressure in the room. If a fan is added to the room, proximity to the patient should be considered to contain contamination near the source.
- Electrical & Med Gas Infrastructure: Medical gas is another obvious deficiency in hotel occupancies. These systems and the storage of bulk materials should be located and protected per NFPA codes and standards to provide safety to surrounding people and structures. If piped oxygen is utilized, a bulk tank, vaporizer, and pipe system should be provided on the site and into the building. Routing this pipe in the corridor and into each space would provide the quickest turn around on construction. If a piped system is not feasible, a bottled oxygen system may be provided. The bottle storage will need to meet the requirements of NFPA and the IFC to safely store the bottles. Electrical infrastructure does not typically include an emergency generator in hotels. This system would need to be provided and integrated as required to maintain a safe environment and critical patient support functions.
CONVENTION CENTER/ARENA/ AUDITORIUM CONVERSIONS
Convention centers and similar high-occupancy venues (enclosed arenas and auditoriums) are well-suited to convert to temporary healthcare facilities or command/control centers. Convention centers by nature are flexible, convertible spaces, and the architectural and systems infrastructure decisions made during design and construction are typically done to provide adaptability for the needs of a yet undefined clientele. There are several components of an urban convention center that might be re-purposed in various ways to suit the needs of the temporary facility.
- Entry/Lobby/Pre-Function: An urban or community focused convention center is most often provided with multiple points of entry at varying corners of the same city block, or perhaps across several city blocks. The entries may be adjacent to bus drop offs, or mass transit, allowing for convenient ambulatory access. If repurposed to a temporary healthcare facility, entries could be zoned or tiered to focus on a particular patient need, relying on signage at the city corners and building exterior to direct the public or emergency personnel to various entry points. One entry point might be family access/registration, another may be emergency responder/staff/private access, and a third could be more medically focused and be configured as a screening/triage station. These spaces are typically open, provided with generous power provisions, and connected to all other portions of the center in such a way that an organized “traffic” pattern could be created from the point of entry to the next stop needed for a particular occupant.
- Restrooms: Convention centers are generally designed (in the large public spaces noted herein) at nominally 7-10 square feet per person, so the accompanying infrastructure must be able to accommodate that density. Large banks of public restrooms are typically accessible from both the public side (lobbies/pre-function) and the event side (exhibit halls) of the facility. While these restrooms aren’t personal or isolated, they do offer needed capacity if isolation is not required.
-
Exhibit Halls: The centerpiece of most convention centers, exhibit halls can be expansive open areas with soaring ceilings, flat floors, and a flexibility that is not available in most other commercial/public spaces. Exhibit halls come in varying sizes and shapes, but as an example, might be a large, 200,000 SF open space that is sub-dividable with air walls into four smaller 50,000 SF spaces. In a conversion to a temporary healthcare facility, each of those sub-dividable spaces could be assigned a different level of acuity.

Exhibit halls are typically provided with access to a loading dock, configured with ramp access for direct drive in, or perhaps accessible via oversized freight elevator. Most access is maintained, even when the halls are sub-divided. Exhibit halls are often provided with an electrical infrastructure that can adapt to whatever need may be present — a common configuration provides utility floor boxes at 30-60 feet on center across the open floor of the exhibit hall. The utility boxes are highly customizable, but often are provided with 100A of power at 208Y/120V — 3 phase. Utility boxes may be provided with water service (though it is generally classified as non-potable), drains, compressed air, and low-voltage (copper/fiber) connectivity. In addition, utility boxes may be provided with a “bail-out” system of empty conduits (perhaps 4-6″) that provide connectivity to each box and out to the loading dock.
Configured as a temporary healthcare facility, the utility boxes would be the “hub” for the electrical needs, with a capacity to serve significant numbers of patient stations, or bed line-ups depending on the configuration. Similarly, the fiber/copper connectivity in each box can be used to create local monitoring and networking capability, as could the presence of Wi-Fi and DAS systems throughout the facility. If a bail-out system is available, it could be used to pull temporary medical gas hoses or water lines from infrastructure located at the loading dock. There is the possibility that if the water connections were all extended above the flood rim of the utility box that the water could be classified as potable and used for local handwashing and sanitation. The HVAC systems are often zoned by divisible space as well, providing some measure of isolation between adjoining rooms, and the occupant density of the spaces typically introduces the need for the HVAC to accommodate significant outside air volumes. In a conversion scenario, the electrical distribution is well-suited to accommodate local exhaust or filtration units as needed to create isolation or necessary pressure relationships, even if the mechanical infrastructure itself may need to be provided.
In some cases, exhibit halls are also outfitted with catwalk systems and “mega columns” that can deliver the same flexibility of services afforded by the utility boxes, perhaps even more so as “bail-out” services could be strung along the cat-walks and dropped down to the areas of the floor where they are needed below.
- Meeting Rooms/Ballrooms: The desired flow of convention centers typically pushes/pulls event attendees from the exhibit halls to smaller breakout or plenary sessions in blocks of meeting rooms or a larger ballroom/multipurpose space. Though smaller in square footage and volume than the exhibit halls, the meeting rooms and ballrooms are designed with the same flexibility and sub-divisibility in mind. Power is generously provided in a combination of floor and wall outlets. Though not typically provided with the same power capacity as the exhibit halls, meeting rooms and ballrooms still generally have permanent power provisions (and temporary power provisions via company switches) to support a multitude of functions in a temporary conversion. Meeting rooms could be dedicated to high- or low-acuity patients, used as command and control space, or perhaps even as a respite zone for staff and emergency personnel. These spaces do not generally have the same ease of access to a loading dock and are typically connected to the dock through the vertical transportation systems. These spaces are often provided with carpet or similar sound absorbing materials on the floor, so provisions might be needed to temporarily remove those materials during a conversion.
- Kitchen/Commissary: Given the frequency of banquet events in convention centers, many are provided with full cooking kitchens and commissaries. The benefit being they are well-suited to provide nutrition and meals to patients, families, and staff/caregivers as needed. Most kitchens/commissaries are connected via back of house service corridors and vertical transportation to the exhibit halls and meeting rooms/ballrooms, allowing for efficient and isolated delivery lanes to all parts of the facility.
- Emergency Power: Convention centers are typically provided with emergency power in the form of diesel generator systems, and most are designed in accordance with Articles 700, 701, and 702 of the National Electrical Code (NEC). However, they generally are designed to support only emergency egress from the facility, not ongoing support of operations, especially for the HVAC systems, and most often only have enough diesel fuel on-site for nominally eight hours of operation or less. The loading docks do afford the opportunity to place mobile/temporary generators at the dock and provide temporary connections to the existing normal services as a means of ensuring continued operations on-site in the event of utility power failure.
Converting existing buildings to serve the healthcare needs of our communities can help alleviate the demand for additional patient beds and isolation rooms. While this may not be easy, we believe that getting our healthcare system the capacity that it needs to meet this challenge is critical to the success of managing this pandemic. Remembering the core purpose of a space will help guide and direct design and construction teams as we dive into creating the best healing spaces possible in a wide variety of locations.
We look forward to doing our part to get started. Let us know if we can help.
ABOUT THE AUTHORS
Jake Katzenberger, Healthcare Technical Leader
As a healthcare technical leader, Katzenberger not only understands how building systems work, but how they integrate with the function of the space. He has personally performed site investigations and managed solutions for more than 75 pharmacies since 2017. Jake leverages 15 years of experience to advance the technical standards of our healthcare practice. Katzenberger combines new technology, design innovation, and lessons-learned to push the firm's healthcare design standards to the next level. He provides direct design oversight, resources, and mentoring to ensure a coordinated, code-compliant, and functional design.
Mark Chrisman, Healthcare Practice Director | Vice President
Mark Chrisman joined Henderson Engineers in 2004 and quickly began establishing client relationships that he still maintains today. A vice president and the firm's healthcare practice director, Chrisman coordinates strategy for Henderson’s healthcare practice across the country. He has designed healthcare environments for some of the biggest names in the industry, providing technical expertise on fire protection and code consulting. He is known for his ability to recall specific codes and uses his knowledge of regulatory compliance requirements to help save clients money and time on projects.
Russ Murdock, Convention Center Practice Director | Vice President
Murdock serves as Henderson’s convention center practice director and has extensive experience designing healthcare and venue facilities. As a vice president, he features a deep understanding of high-occupancy facilities, including their enormous central plants and intricate emergency systems. Murdock has assisted on projects for some of the firm's largest healthcare clients and has an internal drive to make every facility he touches high-quality and high-impact. An avid learner and mentor, this former professor in Kansas State University’s College of Engineering has a passion for helping clients and colleagues reach new heights.
Related Stories
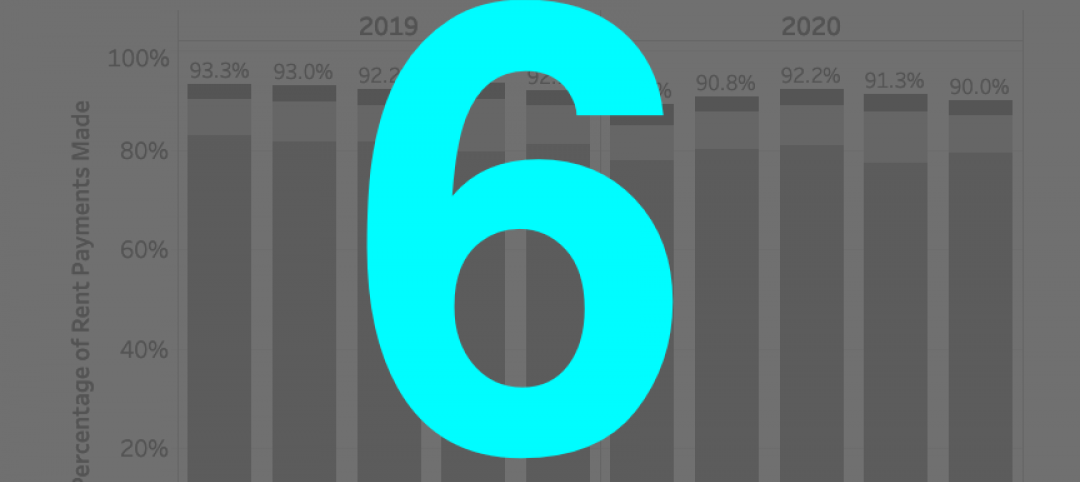
Coronavirus | Aug 25, 2020
6 must reads for the AEC industry today: August 26, 2020
Big-box retailers’ profits surge, and rent payment tracker finds 90% of apartment households paying rent.
Coronavirus | Aug 25, 2020
7 must reads for the AEC industry today: August 25, 2020
Medical office buildings get a boost by demand and capital, and why the COVID-19 pandemic is increasing the need for telemedicine.
University Buildings | Aug 20, 2020
Student housing in the COVID-19 era
Student housing remains a vital part of the student and campus experience.
Coronavirus | Aug 17, 2020
Covid-19 and campus life: Where do we go from here?
Campus communities include international, intergenerational, and varied health-risk populations.
Coronavirus | Aug 10, 2020
Reimagining multifamily spaces in the COVID era
Multifamily developments pose unique challenges and opportunities.
Coronavirus | Aug 3, 2020
Exploring the airborne transmission of the coronavirus and strategies for mitigating risk
Health authorities say it’s important to understand the dangers of microdroplets. How might indoor ventilation need to change?
Coronavirus | Jul 31, 2020
The Weekly show: Microhospitals, mass timber, and the outlook for 5 key building sectors
The July 30 episode of BD+C's "The Weekly" is available for viewing on demand.
University Buildings | Jul 24, 2020
A hybrid learning approach could redefine higher education
Universities reassess current assets to determine growth strategies.
Coronavirus | Jul 20, 2020
Student housing amid the pandemic, infection control in buildings, and future airport design on "The Weekly"
Experts from Core Spaces, Bala Consulting Engineers, and Populous were interviewed in the July 23 streaming program from Horizon TV.