Many healthcare projects on the boards at SmithGroupJJR today will not be finished until the early 2020s. Are we designing buildings that support the way our clients will deliver care on opening day? This is a question my team explored during SmithGroupJJR’s recent Idealab. In the fall of 2016, three teams of architects and planners from across our offices were asked to envision how artificial intelligence (AI) and other advances in technology will shape a healthcare setting in 2025.
My team included Michelle Acosta from our Phoenix office and Stephen Conschafter from our Washington, DC office. We are all planners at SmithGroupJJR, but each of us brought a unique background to this effort. With her training as a health coach, Michelle helped our team explore how AI technology can assist in educating, diagnosing, and even treating consumers at home. A background in urban planning and consulting experience at Deloitte helped Stephen identify the macroeconomic drivers impacting our current healthcare environment. As a recent Master of Health Administration graduate, I used my knowledge of the payment and delivery trends that will shape the healthcare ecosystem of 2025 to provide a context for AI.
Each team was randomly assigned a persona to guide us in developing our design solutions. We were given Peter, a 68-year-old auto assembly plant retiree who lives in the suburbs of Chicago. He is a widower and has a family history of prostate cancer. Peter was a particularly challenging subject for an exercise about the role of artificial intelligence in healthcare: the last time he saw a doctor was for a crown replacement three years ago and he doesn’t like spending money on technology.
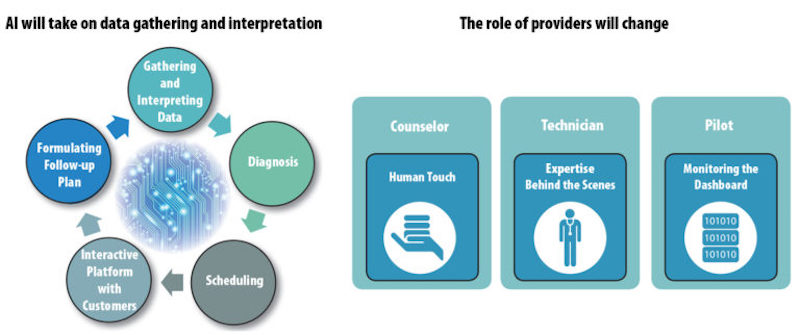
We started our exploration by looking at the role of technology in our lives today. We found a common thread in our dependence on smartphones to track our fitness, shop, find our way around, keep up with the news, stay in touch with other people, etc. In the future, we envision that the smart technology in our phones will be embedded in the items we wear and the objects we use. This exercise brought up a fundamental question: With AI working to gather and analyze the health data from our wearable devices, provide diagnoses, schedule clinical appointments, interact with us, formulate a treatment plan and help us follow it, how will the role of health providers change?
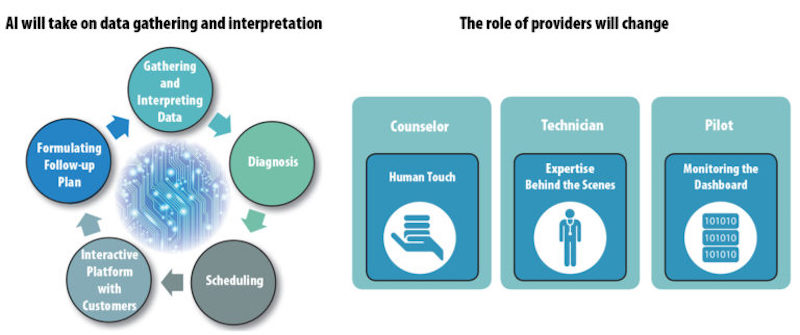
Every member of our team has been a patient at one point or another, and we felt that a human touch at a time when our health fails us and we feel scared and vulnerable will still be important in 2025. Instead of removing the human touch, AI can promote it. In an AI-powered health environment, providers will be able to get a comprehensive dashboard overview of our health status before we show up for an appointment. Equipped with this information, our providers will be able to focus on our person during our visit, rather than on recording our vital signs. The role of staff behind the scenes will also change: the growing complexity of data processing systems will call for expert technical staff that can interact with the AI system.
Peter will be happy to know that in the connected world of 2025, wearables and telemedicine will allow him to take care of most of his health needs without ever setting foot in a doctor’s office. Even Peter’s prostate cancer detection will probably be performed in less complex environments than today. Developments like nanoparticles that can detect cancer and miniature robots that can be ingested and guided from outside a patient’s body will enable procedures that are less invasive than today’s prostate biopsy.
Peter and Medicare have a goal in common: to keep Peter out of the doctor’s office. To contain spiraling costs, the Centers for Medicare & Medicaid Services (CMS) is replacing the old fee-for-service payment model that incentivized providers to give patients more treatments and procedures with payment systems that reward providers for keeping customers healthy and giving them higher quality care instead of a higher quantity of services. Some private payers are also trying to keep members healthy in order to save money; in one example, insurance company Aetna is subsidizing smart wearables that track a patient’s health. This new emphasis on wellness as a way to contain costs will change the way healthcare is delivered in the coming years.
OUR SCENARIO: A PROSTATE BIOPSY IN 2025
We wanted to create a space that embodied the technology and healthcare delivery trends of 2025. Since Peter would not need to visit a provider for any minor ailments, we decided to give him a prostate biopsy. At the beginning of our scenario, the AI system has identified abnormal levels of PSA through Peter’s home biosensor and scheduled a prostate biopsy for him. The biopsy will be performed by a miniature robot that Peter swallows as a capsule. There is no anesthetic and no recovery time. All the clinical aspects of the procedure are invisible.
We considered two AI-powered scenarios for our procedure: one with no human interaction and the other one completely focused on human interaction. In both scenarios, the clinical aspects of Peter’s visit would be entirely hidden. Our first scenario was inspired by Eatsa, an automated San Francisco restaurant where a customer can order food through the internet and pick it up from a cubby, without ever interacting with a person. Our second scenario was inspired by a cruise ship, where a group of travelers share a common experience and are continually catered to by the ship’s staff.
While we were exploring our two scenarios, we ran into an article in the New York Times that talked about the current loneliness epidemic. The article quoted several studies linking loneliness to poor health outcomes. This research inspired us to develop our cruise ship scenario and create a space where Peter can connect with other people as he has his procedure. Today, a prostate biopsy involves going to a urologist’s office, having a needle inserted to extract a tissue sample, and experiencing pain and discomfort for days afterwards. What if, when Peter needs a biopsy in 2025, it could be like shopping at his favorite store, or having a drink with his friends?
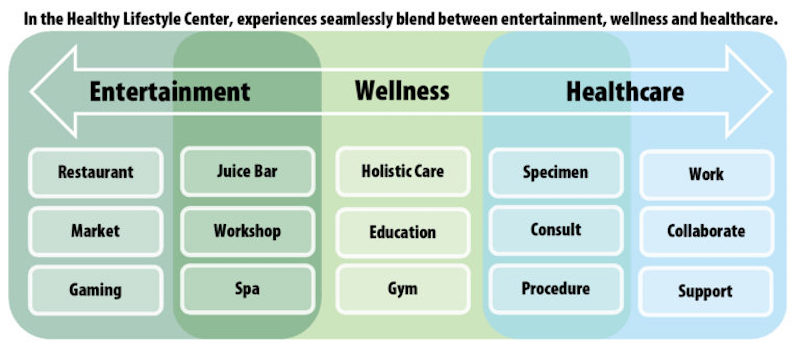
In our cruise ship scenario, Peter’s entire biopsy experience includes human interactions, but nobody is wearing a lab coat. A greeter welcomes Peter as he walks into the clinic and points him to the juice bar. A bartender prepares Peter’s favorite drink and hands him the ingestible robot capsule that will perform his prostate biopsy. Peter can then can decide to go to the barbershop, take a class, watch a movie or just hang out with his friends. Once the procedure is finished, a health coach discusses Peter’s follow-up plans with him and encourages him to join activities at the center.

These interactions happen in a building that promotes healthy lifestyle integration and social interaction, while clinical functions run in the background. Experiences in this environment progress smoothly from retail and entertainment to wellness and health: restaurants and gaming spaces connect to a spa and a gym, and health consultation areas look more like living rooms than exam rooms. Behind the scenes, clinical staff monitor the dashboards of multiple patients, huddle to discuss complex cases, and maintain the AI system.
The increased emphasis on human interaction is enabled by an artificial intelligence quietly humming in the background and gathering Peter’s data, transmitting it to the greeter, stocking the bartender’s fridge with the ingestible robot, and sharing a follow-up plan with Peter’s health coach. In the meantime, Peter is free to choose from a range of healthy experiences that he can share with his fellow customers. And instead of being distracted by data collection, Peter’s wellness team is free to focus on more human connections.
Conclusion
What does the growing payer and provider emphasis on wellness, the proliferation of smart objects, and the emergence of miniaturized procedures mean to us as architects? It means that in ten years, clinics may not need vitals stations and exam rooms to support data gathering, and interventional facilities may not need to accommodate invasive procedures with lengthy recovery times. Instead, we may be asked to create spaces that motivate people to engage in healthy behaviors and that help patients connect to providers and to each other at a human level. The place where Peter gets a procedure may want to look more like Bass Pro Shops or REI than today’s doctor’s office. Now is the time for us to start engaging our clients in conversations about the kinds of buildings they will need in 2025: spaces that leverage the power of artificial intelligence to let people focus on connecting with each other and inspire them to adopt healthy lifestyles.
More from Author
SmithGroup | Mar 28, 2023
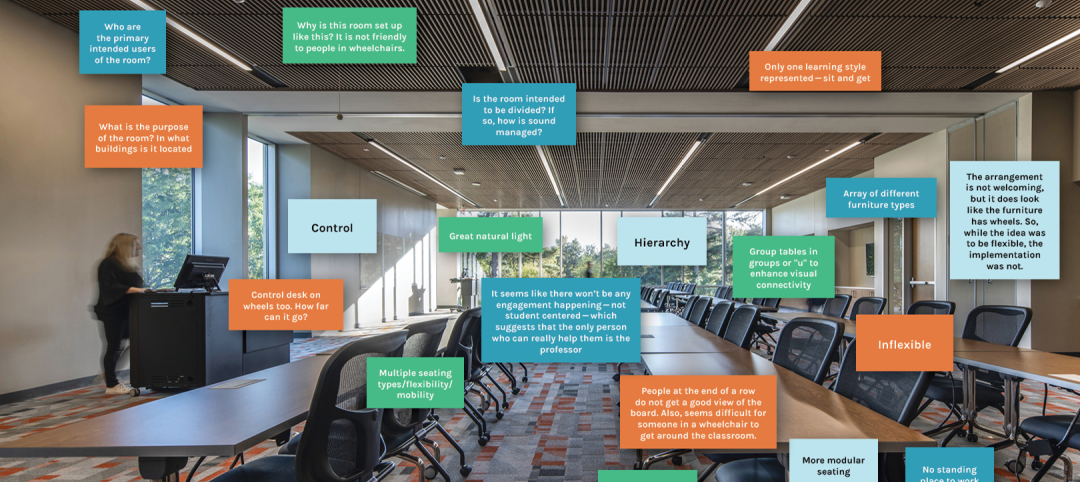
Inclusive design requires relearning how we read space
Pulling from his experience during a campus design workshop, David Johnson, AIA, LEED AP, encourages architects to better understand how to design spaces that are inclusive for everyone.
SmithGroup | Feb 27, 2023
Surfing the Metaversity: The future of online learning?
SmithGroup's tour of the Metaversity gives us insight on bringing together physical and virtual campuses to create a cohesive institution.
SmithGroup | Nov 28, 2022
Data centers are a hot market—don't waste the heat!
SmithGroup's Brian Rener shares a few ways to integrate data centers in mixed-use sites, utilizing waste heat to optimize the energy demands of the buildings.
SmithGroup | Aug 3, 2022
Designing learning environments to support the future of equitable health care
While the shortage of rural health care practitioners was a concern before the COVID-19 pandemic, the public health crisis has highlighted the importance of health equity in the United States and the desperate need for practitioners help meet the needs of patients in vulnerable rural communities.
SmithGroup | Aug 10, 2021
Retail reset: The future of shopping malls
Developers and design partners are coming together to reimagine how malls can create a new generation of mixed-use opportunities.
SmithGroup | May 17, 2021
Future pandemic preparedness at the medical district scale
The current COVID-19 pandemic highlights the concern that we will see more emergency events in the coming years.
SmithGroup | Jan 25, 2021
Amid pandemic, college students value on-campus experience
All the students we interviewed were glad that they returned to campus in one form or another.
SmithGroup | Aug 13, 2020
Renewing the healing role of public parks
While we can’t accurately predict all the ways we will respond to the current COVID-19 pandemic, it should provide a moment of reflection as we see all too clearly the consequences of our exploitation and destruction of nature.
SmithGroup | Jul 21, 2020
How design of senior living communities must change after COVID-19
The cost of maintaining high quality of care and high quality of life for senior living communities has increased up to 73% for senior living communities that remain free of COVID-19 and up to 103% for COVID-19 positive senior living communities.
SmithGroup | Jun 12, 2020
How will museums change after COVID-19
This new environment may herald innovative economic models and change the way we think about museum design.